Don’t remember the lessons on eye anatomy from your highschool biology class? That’s OK—we have provided the following eyeball illustration and terms just to give you a refresher course. And we won’t give you a pop quiz afterwards…
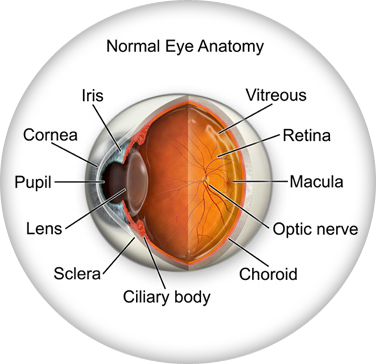
| IRIS | Pigmented tissue lying behind cornea that (1) gives color to the eye, and (2) controls amount of light entering the eye by varying size of black pupillary opening; separates the anterior chamber from the posterior chamber. |
| CORNEA | Transparent front segment of the eye that covers iris, pupil, and anterior chamber, and provides most of an eye's optical power. |
| PUPIL | Variable-sized, circular opening in center of iris; it appears as a black circle and it regulates the amount of light that enters the eye. |
| LENS | Natural lens of eye; transparent intraocular tissue that helps bring rays of light to focus on the retina. |
| SCLERA | The white of the eye; a protective fibrous outer layer covers all of the eyeball except for the part covered by the cornea |
| CILIARY BODY | a muscular ring under the surface of the eyeball; helps the eye focus by changing the len’s shape and also produces aqueous humor |
| CHOROID | The vascular layer between the sclera and the retina; the blood vessels in the choroid help provide oxygen and nutrients to the eye |
| OPTIC NERVE | Largest sensory nerve of the eye; carries impulses for sight from retina to brain |
| MACULA | Small, specialized central area of the retina responsible for acute central vision |
| RETINA | Part of the eye that converts images into electrical impulses sent along the optic nerve for transmission back to the brain. Consists of many named layers that include rods and cones |
| VITREOUS | Transparent, colorless, gelatinous mass; fills rear two-thirds of the interior of the eyeball, between the lens and the retina |
Select from the following list or scroll to learn more about the symptoms and treatments for:
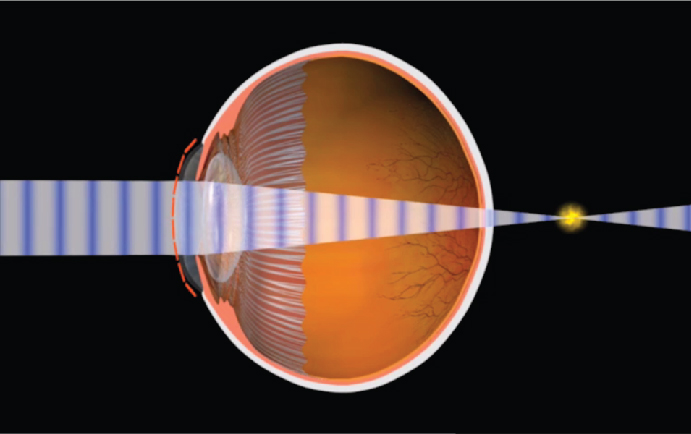
When rays are focused correctly on the retina of a relaxed eye, the eye is said to be emmetropic. Emmetropia is the medical term for 20/20 vision, vision that needs no corrective lenses, contact lenses, or reading glasses. It occurs because the optical power of the eye can perfectly focus an image to the retina, giving it “perfect” vision.
The opposite of emmetropia is ametropia. With ametropia, the focal point of the eye is some distance in front of or behind the retina. The following vision conditions are types of ametropia.
Hyperopia is more commonly known as farsightedness. As the name suggests, people with farsightedness are able to focus on objects that are further away, but have difficulty focusing on objects which are very close. This is because the eyeball is shorter than normal, which prevents the crystalline lens in the eye from focusing correctly on the retina. About a fourth of the population is farsighted. Hyperopia can lead to chronic glaucoma, a more serious condition, later in life.
A family history of hyperopia is a risk factor for developing hyperopia. Babies are often born with hyperopia but they can usually outgrow the condition as their eyes develop into the correct shape.
Hyperopia can be corrected with eyeglasses or contact lenses. There are also new surgical procedures that can correct hyperopia.
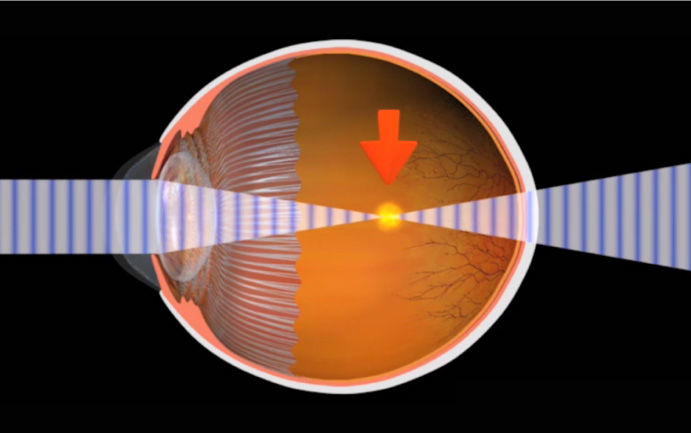
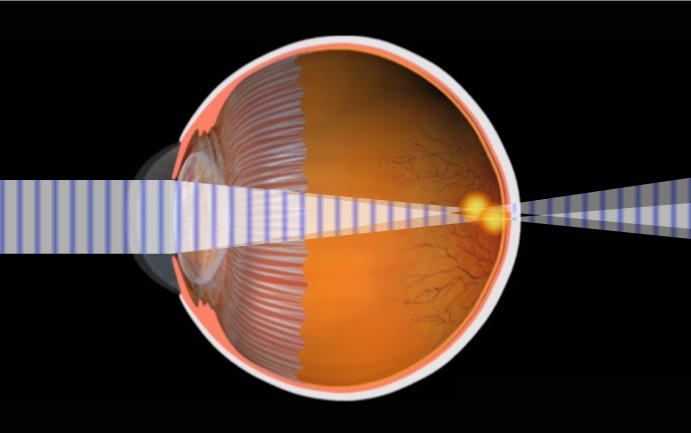
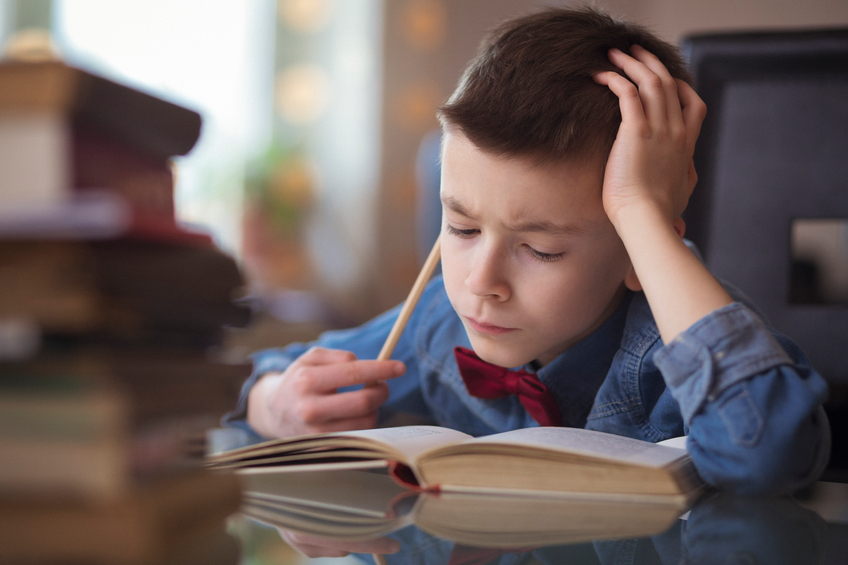
Myopia is the condition of being nearsighted. When it is an inherited condition, myopia begins early in life. People with this condition can usually see near objects, but they struggle to see distant objects. Myopia is the opposite of hyperopia, or farsightedness. In myopia, the anatomy of the eyeball, or globe, is longer than normal. This causes the light to focus in front of the retina, blurring the distance vision. Myopia is corrected with glasses and contact lenses, or with laser vision correction. Laser vision correction is only recommended for people over 18 years old, when the eye has finished growing to adult size.
To correct the symptoms of myopia with glasses, lenses are used that are thicker on the edges and thinner in the middle. This is known as a concave lens, which can be cosmetically improved in higher prescriptions with a high index lens.
Myopes are also at increased risk for a retinal detachment. The signs and symptoms of a retinal detachment are flashing lights, black floaters, or a curtain over the vision. The risk of detachment is typically less than 3 percent.
Amblyopia defined
Amblyopia is also known as lazy eye. It is a condition, usually found in children, in which one or both eyes do not develop properly. An easy way to explain this is that the "eye-brain" connection does not communicate properly; therefore, the child does not know what clear vision is...or what 20/20 vision is. The eye anatomy itself is normal, but the neural pathway to the brain is not normal, causing decreased vision.
Prevalence of amblyopia
Amblyopia is one of the most common treatable forms of vision impairment in children. Its prevalence is as high as 3-5% in some studies. It is most common in infants and young children and it is imperative that this condition is caught early. The chance of successful vision restoration goes down dramatically after age 8, therefore the earlier this condition is caught the better chance of successful treatment.
Causes of amblyopia
The causes of amblyopia are varied. A very common condition that can cause amblyopia is strabismus, a misalignment of the eyes. This occurs when one eye has an abnormal turning in or out, causing the brain to stop using the misaligned eye. Other causes may come from a high prescription such as nearsightedness, farsightedness, or astigmatism. In the case of these conditions, the eye’s vision is out of focus and so the brain turns off that image. Eye disease processes can also cause amblyopia. One of these conditions is known as a cataract. A cataract is a condition of the lens of the eye developing an opacity so that light cannot pass through. Abnormal retinal conditions and hereditary factors can also cause amblyopia.
Treatment of amblyopia
 In order to increase the chances for success, this condition must be detected early. The recommended ages for early eye examination are 6 months old, then 2-3 years of age, and then school age.
In order to increase the chances for success, this condition must be detected early. The recommended ages for early eye examination are 6 months old, then 2-3 years of age, and then school age.
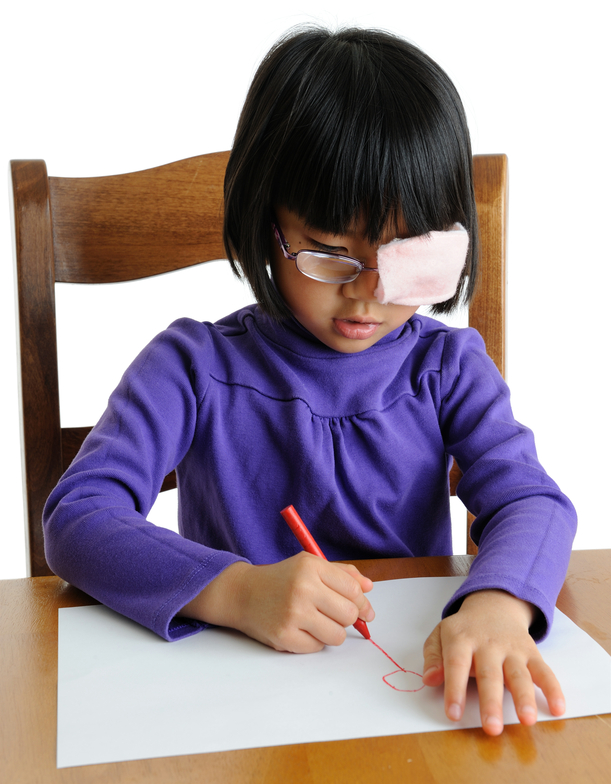
Patching, or occlusion therapy
One of the most common treatments for amblyopia is patching, also known as occluding, the better or stronger eye. This forces the brain to use the weaker eye. An adhesive eyepatch on the skin or a slip-on patch over glasses can be incorporated for occlusion therapy. A blurring contact lens or dilating eye drop can also be used to occlude the good eye.
Surgery
Cataract, eye muscle, or retinal surgery can be incorporated to help treat the underlying cause of amblyopia in some cases.
Vision therapy
Vision therapy has been proven to be successful in the treatment of amblyopia. Vision therapy, or VT, incorporates a series of vision training procedures that helps improve eye movement control, visual acuity, depth perception, and eye coordination. Vision therapy can be done in an office or home setting.
Signs and symptoms of Amblyopia
The most common way amblyopia is diagnosed is a detection of a decreased red reflex in the child's eye. A diagnostic instrument used by the optometrist, ophthalmologist, or pediatrician, can pick up a bright reflection in the normal eye and a dim reflection in the amblyopic eye. Upon further examination, the eye is dilated to see if a refractive error of myopia, astigmatism, or hyperopia is the cause.
Another sign of amblyopia is an eye that turns in or out. A symptom that may be indicative for amblyopia is if the child prefers the vision out of one eye. This can sometimes be detected when occluding the better eye--the child may become fussy and upset because she cannot see out of the lazy eye.
Citations:
1. Amblyopia informational patient brochure. APOS.org. January 2013
As people get older, usually when they hit their 40s, a condition called presbyopia can set in. Presbyopia is the inability to focus on objects near the eye. One usually notices that it is harder to read or use the computer. Bifocals or reading glasses are a way to remedy this condition.
Presbyopia is a natural consequence of the aging process. There is no known cure, though researchers are constantly looking for one. Even if someone has never had vision problems before, he can still develop presbyopia. It may seem to occur suddenly, but it actually occurs over a long period of time. Symptoms include having to hold things at arm’s length to see them clearly, eye strain, fatigue, and headaches from near work.
Sometimes the cornea is irregularly shaped, causing the eye to focus an object on two different areas of the retina. This is known as astigmatism. For the cornea to bend light correctly, it should be dome-shaped, like a basketball. Astigmatic corneas are shaped more like a football. This causes a distorted view when looking at objects which are close-up and far away.
The cause of astigmatism is unknown. Astigmatism is often associated with myopia or hyperopia, and it usually is present from birth. It may be hereditary, or it may be caused by factors such as pressure on the cornea, incorrect posture, or increased use of the eyes for “near work.”
Mild astigmatism usually does not need to be corrected. Eyeglasses, contact lenses, or refractive surgery can correct moderate to high degrees of astigmatism.
Computer vision syndrome (CVS) affects three out of four computer users. It is a series of symptoms related to extended periods of computer usage. Though it is no cause for panic, measures can be taken to relieve symptoms of CVS.
Symptoms
CVS can appear as a variety of symptoms. Headaches, eye strain, neck and back aches, sensitivity to light, blurred vision, double vision, and dry or irritated eyes are all possible problems related to CVS.
Risk Factors
Any computer user can develop CVS. Your vision, your computer, and the environment where you use your computer are all factors which can lead to CVS.
Our top priority is the care of your eyes. We want to keep your eyes healthy through regular eye health evaluations, communication, and education. This page lists a few of the most common eye diseases. Select from the following list of topics or scroll to learn about the causes, symptoms, and treatments for:
There are two types of blepharitis. Seborrheic blepharitis is often part of an overall skin condition called seborrhea, which may also affect the scalp, chest, back and the area behind the ears. The second form of blepharitis – staph blepharitis – is a more severe condition, caused by bacteria, that begins in childhood and may continue through adulthood.
Causes
Hormones, nutrition, general physical condition, and even stress may contribute to seborrheic blepharitis. Build-ups of naturally occurring bacteria contribute to staph blepharitis.
Symptoms
Blepharitis could be described as dandruff of the eyelids. Seborrheic blepharitis results in redness of the eyelids, flaking and scaling of eyelashes, and greasy, waxy scales caused by abnormal tear production. Staph blepharitis can cause small ulcers, loss of eyelashes, eyelid scarring, and even red eye.
Treatment
Careful cleaning of the eyelids can reduce seborrheic blepharitis. Application of hot packs to the eyes for 20 minutes a day can also help. Staph blepharitis may require antibiotic drops and ointments.
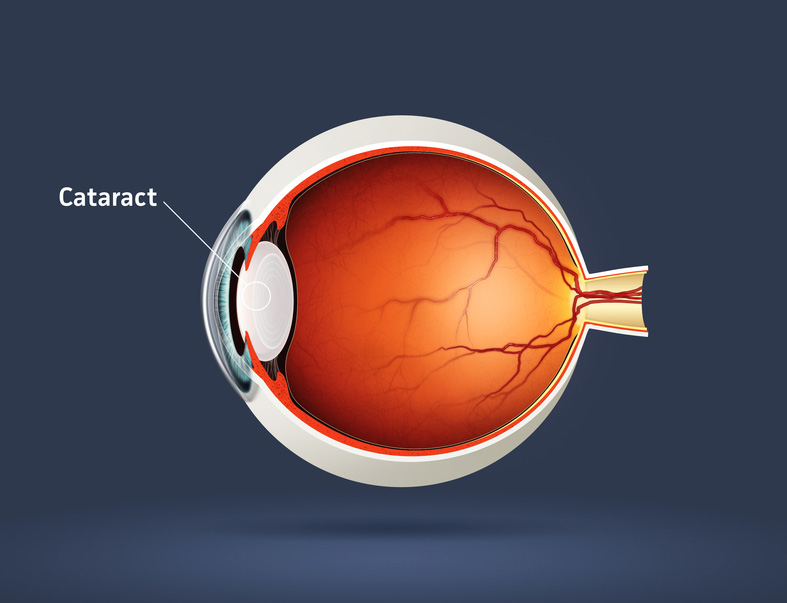
A cataract is an opacity of the lens of the eye. The body's natural lens is similar to an onion, with many layers. These layers contain protein and as the proteins clump together, they cover the lens and make it difficult to see clearly. Cataracts are generally seen in the older population, but they can occur at any age, even birth. By age 60, over half of the population has some symptoms of cataracts due to the natural aging process.
Cataracts are painless but if left untreated can lead to blindness. Cataract surgery is done on an outpatient basis with little or no downtime afterwards. The surgery is performed by a medical doctor known as an ophthalmologist, who specializes in surgery of the eye. The aftercare or postoperative care can be administered by an ophthalmologist or an optometrist.
Symptoms of Cataracts
There can be a myriad of symptoms when a person develops a cataract. It is common for vision to be blurry, as though you are looking through a foggy window. Color vision changes occur in which the brightness of colors fade, especially blue and green. Patients with cataracts also experience difficulty in reading small print. They also feel like they need brighter light or possibly a new glasses prescription. Double vision or vision that seems like halos around the letters also occurs, as well as sensitivity to light.
Causes of Cataracts
The exact physiological cause of cataracts is unknown, but there are many risk factors. Aging and trauma are known to cause cataracts. A blunt trauma or injury to the eye can cause a cataract at any age. The effect of aging on the cells of the lens contributes to cataracts usually after age 60. There is also a direct correlation between the sun's UV rays and certain radiation exposures that contriibute to cataract growth. Smoking is a big risk factor for developing cataracts as well.
Poor nutrition can add to the risk of developing cataracts. Lack of vitamin C has been shown to increase the genesis of cataract formation. Some prescription medicines, especially prednisone, can cause cataracts. Diabetes and other chronic disease processes are also factors in cataract formation. Finally, there are genetic factors that contribute to a cataract.
Treatment of Cataracts
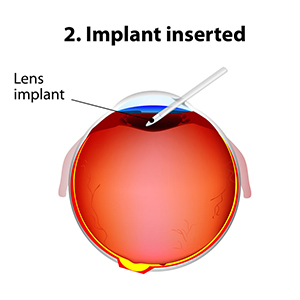
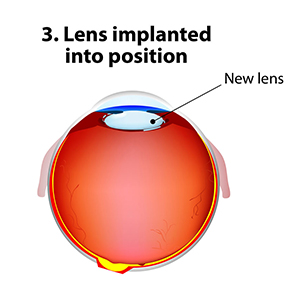
The standard of care for the treatment of cataracts is typically surgery. Cataract surgery, which is an outpatient procedure, removes the protein accumulation from the eye by replacing the cloudy natural lens with an artificial lens. This artificial lens, known as an IOL or intraocular lens, will have your prescription, which in most cases, makes you less dependent on glasses. Lens technology has evolved over the years to also accommodate prescriptions for astigmatism and bifocal prescriptions. Cataract surgery is one of the most commonly performed surgeries in the United States, and it has a success rate of over 98%.
There are many types of cataracts that form on the eye, with different levels of density. This can affect the post-operative care of cataract patients. After cataract surgery, it might be necessary to use a laser to clear an after-cataract membrane that can occur weeks to months after the procedure. This treatment uses a YAG laser and is a painless, low risk, in-office procedure. Most patients can return to work or normal activities within days after the procedure. Your doctor will likely prescribe eyedrops to prevent infection and swelling.
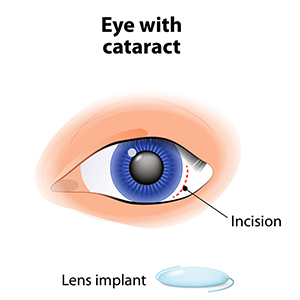
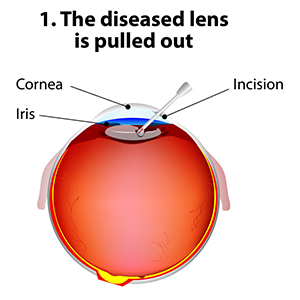
Recent Findings
New technology in cataract surgery includes a bladeless customized procedure that allows for faster healing and clearer vision after the procedure. This computer assisted surgery uses a laser to make the incisions. The laser also divides the cataract efficiently so that the surgeon can remove the old lens and replace it with a new state-of-the-art IOL ( Intraocular lens). This technology uses a femtosecond laser which emits cool pulses of energy. This technology has been used for decades in LASIK surgery for the correction of myopia or nearsightedness. This form of cataract surgery now allows the procedure to be more precise, and reproducible.
Citations
1. What is a cataract? Educational website release. Triadeye.com. January 13, 2013.
2.Bladeless cataract laser surgery. LenSX press release. October 4, 2012.
Conjunctivitis, commonly called pink eye, is a redness of the eye. It is often accompanied by a discharge (clear, yellow, or white) and itching in the eye.
Causes
Pink eye is most often a viral infection, but it can also be caused by bacteria or an allergic reaction. Viral pink eye is highly contagious.
Prevention and Treatment
To avoid spreading conjunctivitis, wash your hands often, do not touch the infected area with your hands, do not share washcloths or towels, and avoid using makeup which may become contaminated. A child with pink eye should be kept from school for a few days. Sometimes an eye doctor will need to prescribe antibiotic eye drops and ointments to clear up conjunctivitis.
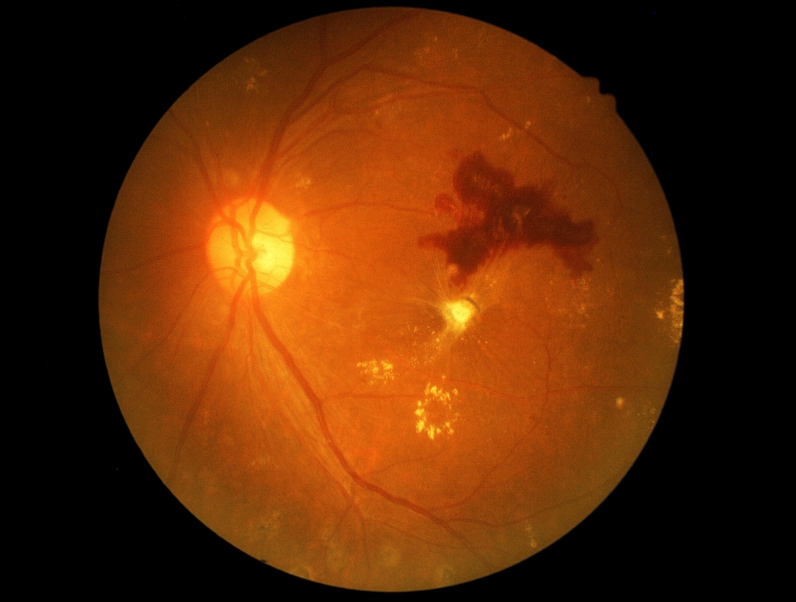
Diabetic retinopathy is a condition associated with diabetes. High levels of blood sugar may damage tiny blood vessels in your eye. New vessels may form to replace the damaged vessels. The new vessels can burst, resulting in blurred vision or even blindness.
Symptoms
Symptoms of diabetic retinopathy include:
- "Floaters” – small specks that pass across your field of vision, made up of cells floating in the transparent gel of your eyeball
- Difficulty reading or seeing things close-up
- Sudden loss of vision
- Flashes
- Blurred or darkened vision
Risk Factors and Treatment
If you have diabetes, make sure you control your blood sugar level. This will reduce your risk of getting diabetic retinopathy. If you are experiencing some of the symptoms listed above, give us a call. If diagnosed properly, diabetic retinopathy can be treated with a laser procedure or a vitrectomy.
If your eyes are constantly itchy or dry, you may have dry eye syndrome, which affects many millions of Americans. Dry eye syndrome is caused by a lack of, or poor quality of, tears. Tears lubricate the outer layer of the eye called the cornea. If the tears are not adequate or are not composed of a proper balance of mucous, water, and oil, the eye becomes irritated.
Symptoms
Dry eye syndrome leads to a number of symptoms, including itchiness, irritation, burning, excessive tearing, redness, blurred vision that improves with blinking, and discomfort after long periods of watching television, using a computer, or reading.
Risk Factors
There are many factors that can contribute to dry eye syndrome. These include dry, hot, or windy climates; high altitudes; air-conditioned rooms; and cigarette smoke. Contact lens wearers, people with abnormally dry skin, and the elderly are more likely to develop dry eye syndrome. You may also be more at risk if you take certain medications, have a thyroid condition, a vitamin-A deficiency, Parkinson’s or Sjorgen’s disease, or if you are a woman going through menopause.
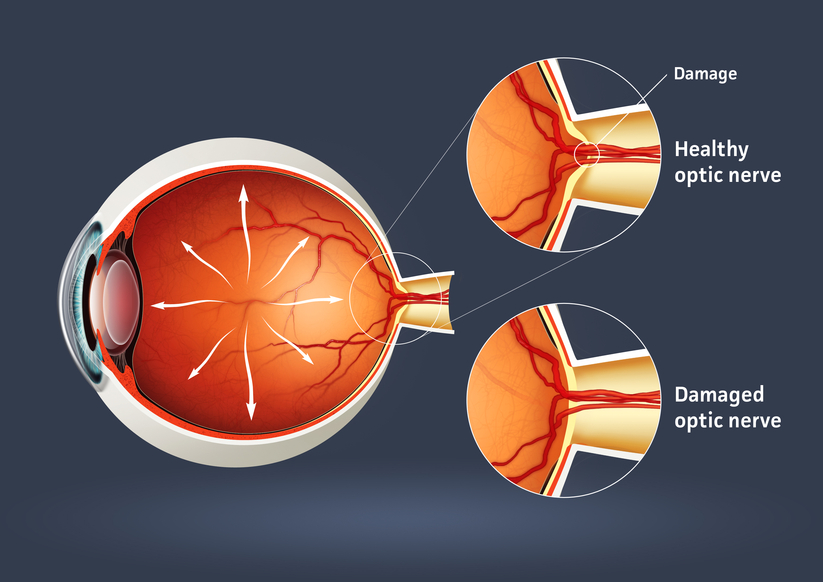
Glaucoma is a serious sight-threatening condition in which there is an abnormal pressure inside the eye. Typically, the pressure or IOP (intraocular pressure) is too high for the blood vessels and optic nerve to function normally, leading to loss of vision.
There are some forms of glaucoma that can occur with normal pressure in the eye. The average IOP for a healthy eye is 10 to 22 mm of Mercury. Just as a physician’s office tests your blood pressure annually, the eye doctor tests your IOP during annual eye examinations.
Types of Glaucoma
There are several varieties of the disease, with primary open-angle glaucoma being the most common. Primary open-angle glaucoma (POAG) occurs when the IOP is higher than normal. As the pressure increases, it destroys vital nerve tissue that is irreparable. POAG usually occurs over a long period of time, months to years, and slowly causes peripheral visual field loss. If left untreated, a sufferer progresses to tunnel vision and then to total blindness.
A second type of glaucoma is acute-angle closure. This is considered a medical emergency because the interocular pressure spikes suddenly to anywhere from 30-70 mm or higher. This causes extremely sharp pain, nausea and vomiting, and cloudy vision. The IOP needs to be lowered within hours to prevent permanent vision loss.
Juvenile open-angle glaucoma, or JOAP, is similar to POAG, in that is causes a gradual visual field loss. The most common form is in children from ages 3 to 21. Infantile or congenital glaucoma is a type of glaucoma that manifests itself between birth to 3 years of age. A typical sign is an enlarged bluish-gray cornea, the front dome of the eye. Excessive tearing of the eye and sensitivity to light are also symptoms. Finally, secondary glaucoma is caused from trauma, eye disease, or certain medications.
Causes of Glaucoma
Many theories on the cause of glaucoma exist, but the exact cause is unknown. Glaucoma can be a hereditary condition. It also can be caused by malformed anatomical structures in the eye. Certain risk factors such as hyperopia and cataracts cause a higher incidence of certain types of glaucoma.
One cause of glaucoma is an insufficient drainage system of the aqueous fluid. The aqueous imbalance causes a gradual buildup of pressure which destroys vision. Another cause is an insufficient flow of blood to the optic nerve. Ocular trauma or injury that damages the anterior segment for the lens and drainage mechanism of the eye can also lead to glaucoma. In the case of normal tension glaucoma, pressure readings are in the normal range. The cause of this is unknown.
Treatment
Even though in most cases there is no way to prevent glaucoma, there are many treatment options. Medications in the form of eyedrops are commonly prescribed. Different combinations of agents act on mechanisms of action to lower IOP or to slow the production of fluid.
Advanced surgical and laser procedures can also be viable options for the treatment of glaucoma. An in-office procedure called laser trabeculoplasty can cause the meshwork in the eye to work more efficiently. This treatment has a temporary effect and may need to be done multiple times. Another effective surgery uses a drainage implant to facilitate better outflow and inflow of aqueous fluid in the eye. These procedures help keep the pressure stabilized. Conventional surgery for glaucoma is done in an operating room scenario. A flap in the eye is created to facilitate outflow of the pressure. This pressure-controlling surgery is known as a trabeculotomy.
Furthermore, some oral medications can also be used in the treatment of glaucoma.
Methods of Testing for Glaucoma
During a comprehensive eye examination, eye pressure can be tested through various methods. Tonometry gives a pressure reading of the eye. A tomometer has different methods such as a probe that gently touches the front of the eye after the eye doctor has administered anesthetic eyedrops. Another method of testing uses a puff of air. For children, there is a tonometer that is quick and does not require anesthesia.
A pachometer, which measures the thickness of the front of the eye called the cornea, can also aid in diagnosis. A visual field device can measure for early or late damage in the peripheral fields of vision. Lastly, newer technology called OCT, or optical coherence tomography, counts the nerve fibers, which can help detect early changes in the disease.
Prevalence of Glaucoma
There are approximately 3 million individuals in the United States with glaucoma. It is the second leading cause of blindness in the country. Most cases are found in the population over age 40, and more women than men have the disease. Two thirds of glaucoma cases are in the Caucasian population, approximately 20% are African-American, and 10% are Hispanic. Glaucoma continues to rise every year in the population.
The key to success in the treatment of glaucoma is early detection and progressive monitoring of the condition. Comprehensive eye examinations and diligent monitoring will help protect from vision loss with this disease.
Citations
- Glaucoma. AOA pdf. AOA.org.
- I Care Tonometry in Children. JAAPOS. Sciencedirect.com. April 2011
- Glaucoma, open -angle. NEI source press release. 2010.
Macular degeneration is a disease which affects a small area of the retina known as the macula. The macula is a specialized spot on the retina that allows us to see the fine detail of whatever is directly in front of us. Macular degeneration occurs when the macula begins to deteriorate.
“Wet” vs. “Dry”
Most often, macular degeneration is accompanied by formation of yellow deposits, called “drusen,” under the macula, which dry out or thin the macula. This is called “dry” macular degeneration. In rare cases, abnormal blood vessels develop under the macula and leak fluid. This is called “wet” macular degeneration.
Causes
A number of uncontrollable factors contribute to macular degeneration, including age, sex, eye color, farsightedness, and race. Risk factors you can control include smoking, high blood pressure, exposure to harmful sunlight, and diet.
Symptoms
It is difficult to detect dry macular degeneration in its early stages. The most common symptoms, when detected, include a spot of blurry vision, dark vision, or distorted vision. Wet macular degeneration progresses much faster than the dry variety. Both forms of macular degeneration can cause blindness.
Treatment
Currently, there is no cure for macular degeneration, but treatment is available to slow the effects.
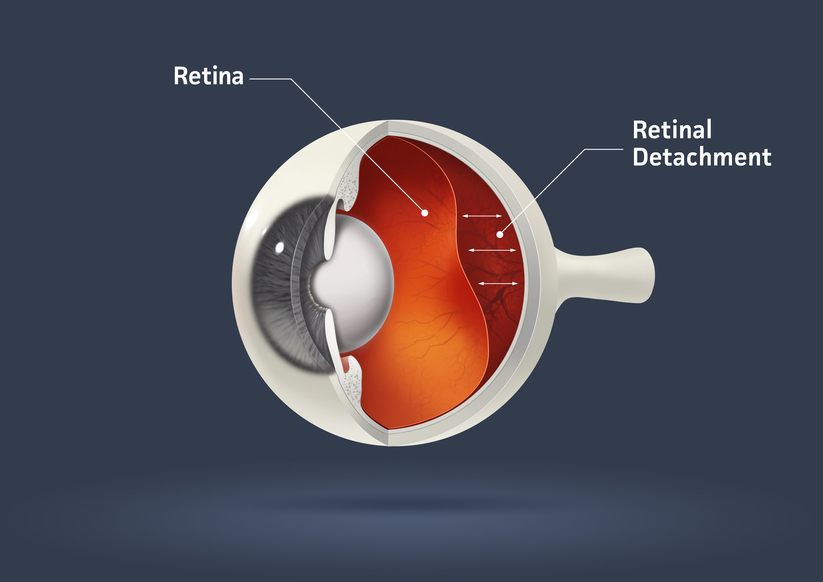
The part of the eye which collects light and transmits the light messages to the optic nerve and brain is the retina. It lines the inner back wall of the eye. When the retina separates from the back wall, it is known as retinal detachment. It is a serious condition which can cause permanent damage and vision loss if not treated quickly.
Symptoms
A retinal detachment often causes sudden defects in your vision. It may just cause a blind spot too small to notice, or it may cause a noticeable shadow which obscures your vision. An increase in “floaters,” which look like small particles or fine threads, may also be noticed. Finally, flashes of light are associated with retinal detachment.
Risk Factors
Eye injuries, tumors, and cataract surgery can cause retinal detachment. Nearsighted individuals and the elderly are at greater risk for spontaneous detachment. Also, diabetic retinopathy, a condition associated with diabetes, can cause bleeding which leads to retinal detachment.
Presbyopia is a Latin term for "old man eyes." This condition actually begins in your late 20s and slowly causes close vision loss. Most people develop symptoms after age 35--these symptoms include eyestrain and blurry vision while reading. Often presbyopia causes people to push objects further away to view them clearly. The treatment for presbyopia includes glasses and contact lenses, laser procedures, and other surgical procedures.
Reading glasses, bifocals, trifocals, or progressive multifocal blended lenses are all options to treat and correct presbyopia with glasses.
Soft, rigid, gas permeable, or a combination of these materials can treat presbyopia with contact lenses. Many surgical and laser techniques are used to treat presbyopia with new technology developing every year for this emerging population.
To reduce eye strain and fatigue, we carry specialized computer lenses. These lenses are perfect for computer users who spend a majority of their days working on computers. And since three out of four computer users will suffer from Computer Vision Syndrome, computer lenses are a great way to keep your eyesight healthy.
One of the first areas of your life where presbyopia becomes prominent is in your ability to read. There are a variety of styles available, with sleek designs that allow you to carry them anywhere.
For many presbyopes, bifocal lenses are a necessity. But it can be difficult to adjust to the harsh line that is found in many bifocal lenses. Fortunately, there are no-line lenses, which are also called progressive lenses. No more lines! Just a change in focusing power which allows you to comfortably focus on any distance. Just as with lined bifocals, distant objects are viewed through the top portion of the lenses, and near objects are viewed through the bottom portion of the lenses.
If you need bifocals but cannot stand wearing glasses, you may need bifocal contact lenses. Now you can have all of the benefits of bifocal lenses in the convenience of contact lenses. Talk with your doctor about bifocal contacts today.
For some of our emerging presbyopes we offer another option to glasses. Monovision is a method of fitting your dominant eye for distance vision and your non-dominant eye for near vision. Contacts are available in disposable, extended wear, and even daily disposable lenses to fit your lifestyle. Most patients require 2-4 weeks to make the adjustment from binocular vision to monovision.
Children with uncorrected vision conditions or eye health problems face many barriers in life, academically, socially, and athletically. High-quality eye care can break down these barriers and help enable your children to reach their highest potential. As a parent, make sure you are giving your children the eye care they need. Presented are guidelines from the American Optometric Association.
Your baby has a whole lifetime to see and learn. But did you know your baby also has to learn to see? As a parent, there are many things that you can do to help your baby’s vision develop.
When your baby is about six months, you should take him to your doctor of optometry for his first thorough eye examination. Things that the optometrist will test for include excessive or unequal amounts of nearsightedness, farsightedness, astigmatism, lack of eye movement ability, as well as other eye health problems. These problems are not common, but it is important to identify children who have them at this stage. Vision development and eye health problems can be more easily corrected if treatment is begun early.
Unless you notice a need, or your doctor of optometry advises you otherwise, your child’s next eye exam should be around age three, and then again before he or she enters school.
During the first four months of life, your baby should begin to follow moving objects with the eyes and to reach for things, first by chance and later more accurately, as hand-eye coordination and depth perception begin to develop.
To help, use a nightlight or other dim lamp in your baby’s room; change the crib’s position frequently and your child’s position in it; keep reach-and-touch toys within your baby’s focus, about eight to twelve inches from his eyes; talk to your baby as you walk around the room; alternate right and left sides with each feeding; and hang a mobile above and outside the crib.
Between four and eight months, your baby should begin to turn from side to side and use her arms and legs. Eye movement and eye/body coordination skills should develop further and both eyes should focus equally.
Enable your baby to explore different shapes and textures with his or her fingers; give your baby the freedom to crawl and explore; hang objects across the crib; and play “patty cake” and “peek-a-boo” with your baby.
From eight to twelve months, your baby should become mobile, crawling and pulling himself or herself up. He or she will begin to use both eyes together to judge distances and grasp and throw objects with greater precision. To support development do not encourage early walking – crawling is important in developing eye-hand-foot-body coordination; give your baby stacking and take-apart toys; and provide objects your baby can touch, hold and see at the same time.
From one to two years, your child’s eye-hand coordination and depth perception will continue to develop and he or she will begin to understand abstract terms. Things you can do are to encourage walking; to provide building blocks, simple puzzles and balls; and to provide opportunities to climb and explore indoors and out.
There are many other affectionate and loving ways in which you can aid your baby’s vision development. Use your creativity and imagination. Ask your doctor of optometry to suggest other specific activities.
During the infant and toddler years, your child has been developing many vision skills and has been learning how to see. In the preschool years, this process continues as your child develops visually guided eye-hand-body coordination, fine motor skills, and the visual motor skills necessary to learn to read.
As a parent, you should watch for signs that may indicate a vision development problem, including a short attention span for the child’s age; difficulty with eye-hand-body coordination in ball play and bike riding; avoidance of coloring and puzzles and other detailed activities.
There are everyday things that you can do at home to help your preschooler’s vision develop as it should.
These activities include reading aloud to your child and letting him or her see what you are reading; providing a chalkboard, finger paints and different shaped blocks and showing your child how to use them in imaginative play; providing safe opportunities to use playground equipment such as a jungle gym and balance beam; and allowing time for interacting with other children and for playing independently.
By age three, your child should have a thorough optometric eye examination to make sure your preschooler’s vision is developing properly and there is no evidence of eye disease. If needed, your doctor can prescribe treatment including glasses and/or vision therapy to correct a vision development problem.
Here are several tips to make your child’s optometric examination a positive experience:
- Make an appointment early in the day. Allow about one hour.
- Talk about the examination in advance and encourage your child’s questions.
- Explain the examination in your child’s terms, comparing the E chart to a puzzle and the instruments to tiny flashlights and a kaleidoscope.
Unless recommended otherwise, your child’s next eye examination should be at age five. By comparing test results of the two examinations, your optometrist can tell how well your child’s vision is developing for the next major step. . .the school years.
A good education for your child means good schools, good teachers and good vision. Your child’s eyes are constantly in use in the classroom and at play. So when his or her vision is not functioning properly, learning and participation in recreational activities will suffer.
The basic vision skills needed for school use are:
- Near Vision. The ability to see clearly and comfortably at 10-13 inches.
- Distance Vision. The ability to see clearly and comfortably beyond arm’s reach.
- Binocular coordination. The ability to use both eyes together.
- Eye movement skills. The ability to aim the eyes accurately, move them smoothly across a page and shift them quickly and accurately from one object to another.
- Focusing skills. The ability to keep both eyes accurately focused at the proper distance to see clearly and the ability to change focus quickly.
- Peripheral awareness. The ability to be aware of things located to the side while looking straight ahead.
- Eye/hand coordination. The ability to use the eyes and hands together.
If any vision skills are lacking, your child will have to work harder. This can lead to headaches, fatigue, and other eyestrain problems. As a parent, be alert for symptoms that may indicate your child has a vision or visual processing problem. Be sure to tell your optometrist if your child frequently:
- Loses his place while reading.
- Avoids close work.
- Holds reading material closer than normal.
- Tends to rub his eyes.
- Has headaches.
- Turns or tilts head to use one eye only.
- Makes frequent reversals when reading or writing.
- Uses finger to maintain place when reading.
- Omits or confuses small words when reading.
- Consistently performs below potential.
Since vision changes can occur without you or your child noticing them, your child should visit the optometrist at least every two years, or more frequently if specific problems or risk factors exist. If needed, the doctor can prescribe treatment including eyeglasses, contact lenses, or vision therapy.
Remember, a school vision or pediatrician’s screening is not a substitute for a thorough eye examination.
Never overlook the importance of safety eyewear when playing sports. Every year, hundreds of men, women, and children are injured while playing sports. To help prevent sports-related eye injuries, athletes should use protective athletic eyewear whether or not prescription eyewear is needed. One choice is a sports frame with prescription or non-prescription polycarbonate lenses. Baseball or softball players who are hit in or near the eye, or suffer a blow to the head, should seek immediate care at a hospital emergency room or from an eye care professional.
The important thing to remember for parents of children who wear contact lenses is that contacts are prescribed medical devices. Contact lenses are not a cosmetic accessory. While the wearer may be happy about his or her new look, it is extremely important that the lenses be properly cleaned and worn according to the instructions of the optometrist.
- My Child Is Near-Sighted. Will Glasses Correct His/Her Learning Problem?
- What Is the Relationship between Eye Muscle Problems and Learning?
- My Child Loses His/Her Place. Is That Related to the Eyes?
- My Child Reverses Letters and Words. Does He See Backwards?
- What Are the Other Visual Components Necessary for Academic Achievement?
There is controversy over the exact relationship between vision and learning. For example there is a negative correlation between distance refractive error and reading ability. Myopic or nearsighted children who cannot see clearly at a distance without glasses are more commonly good readers. Children who spend tremendous amounts of time reading become nearsighted. Before Alaska became a state myopia was rare. After becoming a state, more than 50 percent of the children in Alaska developed nearsightedness. Thus, correlation is such that nearsightedness or poor distance vision is highly correlated with success in reading. Restated another way, poor distance vision is associated with better reading abilities. Farsighted children statistically are poorer readers than myopic children.
Some of the mechanical visual skills which are related to reading include focusing or accommodation, and eye teaming, or convergence. Fatigue of one or both of these systems may interfere with reading. There is also a relationship between eye movements such as saccades (whereby we change fixation from one target to the next) and smooth following movements known as pursuits and reading. Children who cannot make accurate eye movements are often found to skip lines and words while reading.
The visual system was originally designed so that the peripheral vision was responsive to motion detection (danger from the jungles) with a central portion for fine discrimination (to identify the source of danger; e.g., a lion.) In the school environment the child is expected to ignore the peripheral portion of their visual system and pay attention with the central portion. If the child can not ignore the peripheral portion, he/she becomes distracted. Improvement in eye movement skills often results in less distraction and fewer errors of skipping words while reading.
Reading requires very accurate saccadics, which are fixations from one spot to another. Children who have poor eye movements are easily distracted and lose their place. Remember, the eye movement system was designed so that peripheral vision detects motion and danger. Imagine what happens when the system works correctly in the class room. As soon as there is peripheral movement, the eyes move toward the source of movement. This results in the complaint of inattention. Thus, reflexive eye movement skills must be socialized so that they do not respond reflexively to peripheral information. In addition, speed and accuracy must be trained so that one does not lose one’s place.
The skills are easily improvable with vision therapy. Once the information is brought into the eyes, it must be sent back to the brain for appropriate processing. The information must be utilized and integrated with the sensory and motor areas of the brain. Defects in the perceptual (interpretation of visual system) and motor (the integration with output, e.g., hand-eye coordination) may interfere with the reading process. Perceptual motor skills are key in the early acquisition of reading skills. A deficit is important to identify very early on-- i.e., five to seven years of age. Remediation of the skills at a later date, such as age 12, will be less effective for reading. Thus, early identification and treatment is essential. It is evident that there is more to good vision than 20/20.
It has been presumed that children who reverse letters or words see them backwards. This is false. They have directional confusion. In the real world direction has no meaning. For example, a chair is a chair no matter which way it is placed. Changing direction does not change interpretation. In the world of language direction changes meaning. Connect the bottom of a chair and it looks like a "b". Turn it 180 degrees it becomes a "d", flip it upside down and it becomes a "q" and flip it again it becomes a "p". Thus, direction changes meaning. The difference between "was" and "saw" is direction.
As mentioned previously, we should correct all optical errors of the eyes (glasses); eliminate eye muscle problems; and create smooth accurate eye movements. In addition, we should make sure that we properly interpret what we see and use it appropriately. These are known collectively as perceptual skills and include form perception, size and shape recognition, visual memory, and visual motor integration (hand-eye coordination.)