Location & Hours
4008 Red Cedar Dr D-1
Highlands Ranch, CO 80126-8152
| Mon & Fri: | 8 - 4 |
| Tues - Thurs: | 10 - 7 |

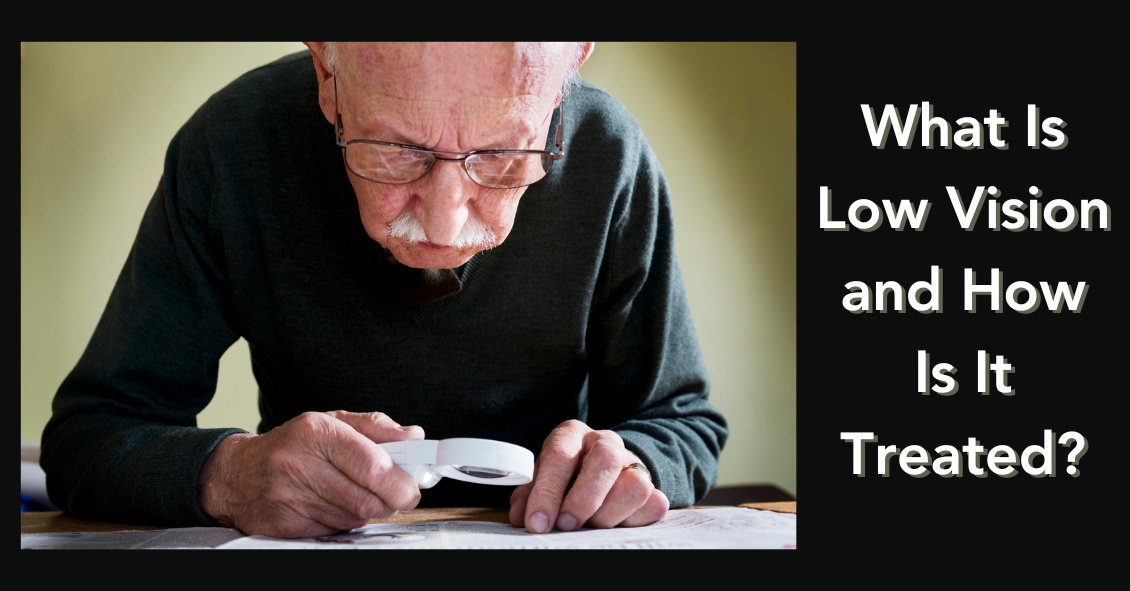
Recent Census Bureau data shows a population of approximately 71 million baby boomers (the generation born from 1946-1964). What does that have to do with low vision you may ask? Approximately 40 million people worldwide have some sort of blindness, and aging increases the incidence of macular degeneration and other vision impairment that qualifies them as “low vision” persons.
Low vision is a condition of the eye in which the vision falls below 20/70 in the better seeing eye. It impairs the recipients, rendering them unable to perform daily tasks that others take for granted. With this rising aging population, the awareness of low vision therapy, diagnosis, and treatments are more widely available.
Low vision treatment can help people recover from decreased visual function due to retinal disease, brain injury, neurological damage, and other causes.
It is not only the elderly population that is affected--approximately 20% of low vision patients are children under the age of 18. Childhood genetic disorders of the eye such as retinitis pigmentosa, albinism, Bests disease, ROP, rod/cone disorders, and glaucoma are among the causes of low vision in the pediatric population.
What can be done to help these millions?
There are eye care practitioners that specialize in low vision, as well as therapists. They train the patient to adjust their current lifestyles to make them more independent and utilize the current salvageable vision they do have. For example, if a person has lost their central vision due to macular degeneration, they can be trained to use their peripheral vision to accommodate for many tasks.
Because patients with low vision cannot be corrected with regular eye glasses, the use of telescopes, magnifiers, computer generated aids, training, biofeedback, and optical magnification devices are among some of the resources available to help. Occupational therapists also employ orientation and mobility assistance to help patients in their daily living skills.
There are many technologies that help to improve vision. One such technology is a bionic eye device that uses a pair of glasses with a camera that transmits video data to an implant in the back of that patients eye (the retina). This device uses technology similar to cochlear implants that stimulate auditory nerve signals to restore hearing. In the same way, visual impulses can be restored by stimulating neurons in the retina, brain, or optic nerve.
Maybe the Bionic Man TV series wasn’t too far out there and can someday be a reality............restoring vision to millions.
For more valuable information on low vision visit:
American Occupational Therapy Association AOTA
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Getting your eyes dilated can be inconvenient – dilation makes your eyes light sensitive, which can make it difficult to read books or use phones and computers for a few 4 hours.
So wouldn’t it be great to have another drop to reverse the effects of dilation?
On Dec. 31, 1990, dapiprazole, under the trade name Rev-Eyes, was approved by the FDA and thought to be the answer to all the post-dilation problems. It was marketed for treatment of medically-induced dilation by stimulating pupillary constriction and restoration of accommodative function for reading.
In clinical practice, dapiprazole took between one to two hours to return pupils to pre-dilation size.
Side effects such as stinging upon instillation, conjunctival hyperemia (redness of eye), headache, and a few instances of ptosis (lid drooping), with a possible additional dollar cost to patients, seemed to lessen dapiprazole’s overall clinical benefit.
Reading ability returned in approximately 43 minutes with dapiprazole vs 66 minutes without the drop (Optom Vis Sci 1994 May; 71(5):319-22). The main complaint that people had after using dapiprazole was the conjunctival hyperemia, which lasted more than three hours. The other issue was that dapiprazole was costly, so some practitioners included an additional charge for the reversal of dilation to offset the cost.
The full adverse reaction profile according to Drugs.com is as follows:
"Adverse Reactions: In controlled studies, the most frequent reaction to dapiprazole was conjunctival injection lasting 20 minutes in over 80% of patients. Burning on instillation of dapiprazole hydrochloride ophthalmic solution was reported in approximately half of all patients. Reactions occurring in 10% to 40% of patients included ptosis, lid erythema, lid edema, chemosis, itching, punctate keratitis, corneal edema, browache, photophobia and headaches. Other reactions reported less frequently included dryness of eyes, tearing and blurring of vision."
Currently, Rev-Eyes is off the market. The FDA has stated that Rev-Eyes was not withdrawn from the market for reasons of safety or effectiveness.
At this time, there is nothing available for reversal of dilation. People who get dilated will still need to wear their sunglasses and to put off reading for a couple of hours until the effects of the dilation drops wear off.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
We are frequently asked if it’s wise to have cataract surgery if you have Macular Degeneration.
Let’s start with some background.
- Cataracts and Age-related Macular Degeneration (AMD) are both leading causes of visual impairment in the elderly population.
- Cataracts develop when the normal clear lens gets cloudy with age. This is correctable with cataract surgery, which involves replacing the cloudy lens with a clear, artificial lens.
- While cataracts affect the front part of the eye, AMD causes damage to the retina, which is the inner back lining of the eye.
There have been concerns about cataract surgery causing progression of AMD. It has been thought that there was an inflammatory component to AMD and the normal inflammatory response after cataract surgery may lead to AMD progression.
But studies have looked at patients who underwent cataract surgery compared to patients who didn't have cataract surgery and the progression of AMD was not significantly different between the two groups. However, those patients with AMD who underwent cataract surgery had a significant improvement in vision.
AMD patients can further be characterized as having wet or dry AMD, and only those with wet AMD require treatment. Patients with wet AMD need injections to decrease the growth of new blood vessels and reduce fluid in the retina.
A 2015 study showed that after cataract surgery, there was an increase in fluid in the retina of patients with wet AMD. Therefore, in patients with wet AMD, we usually want the wet AMD to be stabilized before the patient has cataract surgery. Sometimes an injection may be given prior to cataract surgery to prevent any inflammatory changes that may be associated with cataract surgery.
The majority of the studies on the subject conclude that it is relatively safe to have cataract surgery even if you have AMD and in most cases there is a significant improvement in vision. Removing the cloudy lens also helps the ophthalmologist to better monitor the status of the AMD. You will want to have a candid discussion with your eye doctor on the timing, benefits, and potential risks of cataract surgery with macular degeneration.
Article contributed by Dr. Jan Pan.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Mark your Calendars!!! On Monday, April 8, a solar eclipse will be visible across the entire continental United States and most of Canada.
A solar eclipse occurs when the moon blocks any part of the sun, and with this one, the vast majority of North America will experience at least a partial eclipse.
A lucky few million people along a path from Texas to Kentucy to Ohio to Maine and eastern Canada will experience a brief total eclipse when the moon completely blocks the sun for up to 4 minutes. During this time, it will look like dusk along that path.
This total eclipse will make the solar corona visible, and stars and the planets may also be visible during this time.
But looking directly at the sun before it is completely covered is unsafe. Although there is a limited chance of eye damage if you are in the proper area during the total eclipse it is not worth the risk of retinal damage to even take a quick look at the eclipse if it is not “total.”
A large part of the country is not along the pathway where the eclipse will be total so you should not, and residents should never look at the sun without protection.
The only safe way to look directly at the eclipse is through special solar filters, such as “eclipse glasses” or hand-held solar viewers.
Ordinary sunglasses, even if they are very dark and polarized, are not safe for looking at the sun. You will want to make sure that your eclipse glasses and handheld solar viewers meet the ISO 12312-2 international standard for such products.
Even if you have ISO 12312-2 eclipse glasses, you MUST follow the instructions to keep your eyes safe. Always supervise children using solar filters.
A couple specific instructions are found below, courtesy of NASA’s eclipse website-- https://science.nasa.gov/eclipses/future-eclipses/eclipse-2024/safety/. For complete instructions, read the entire NASA page.
"Except during the brief total phase of a total solar eclipse, when the Moon completely blocks the Sun’s bright face, it is not safe to look directly at the Sun without specialized eye protection for solar viewing.
Viewing any part of the bright Sun through a camera lens, binoculars, or a telescope without a special-purpose solar filter secured over the front of the optics will instantly cause severe eye injury."
A solar eclipse is one of nature’s grandest spectacles. By following these simple rules, you can safely enjoy the view and be rewarded with memories to last a lifetime. An eclipse is a rare and striking phenomenon you won't want to miss, but you must carefully follow safety procedures. Don't let the warnings scare you away from witnessing this singular spectacle! You can experience the eclipse safely, but it is vital that you protect your eyes at all times with the proper solar filters. No matter what recommended technique you use, do not stare continuously at the sun. Take breaks and give your eyes a rest! Do not use sunglasses: they don't offer your eyes sufficient protection. One excellent resource for safe solar eclipse viewing is here: https://science.nasa.gov/eclipses/safety.
The solar eclipse is a spectacular sight but please remember to watch it safely.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
- Why did the guy try to avoid eye surgery by rubbing ketchup in his eyes? He had heard that Heinz sight was 20/20.
- Patient: “Doc, I get a stabbing pain in my eye every time I take a sip of coffee." Doctor: “Have you tried taking the spoon out of the mug?"
- What do you call a penguin with no eye? A pengun!
- At what elevation is your vision the best? See Level.
- Why don’t optometrists use tape measures? They’re really good at eyeballing it.
- What did the eyeball say to the eyelid? "I wish you wouldn't keep me in the dark!"
- Why did the pirate walk into the bar? He had his patch on the wrong eye.
- Cop: “Let me know if you see the suspect with one eye.” Bystander: “I already saw him run that way, but I was using both my eyes.”
- Man 1: “I stopped seeing my girlfriend two days ago.” Man 2: “Really? What happened?” Man 1: “She accidentally poked me in the eyes.”
- Woman 1: “I used to date a man with a lazy eye.” Woman 2: “Why did you stop?” Woman 1: “He was seeing someone on the side.”
- Patient: “Doc, my eyes are really dry.” Eye Doctor: “Here, smell this onion.” Patient: “That made me cry!” Eye Doctor: “Great, I pulled out the onion to make you moist-your-eyes.”
- How are your eye doctor and your teacher the same? They both spend their days testing pupils!

There are many things that can cause your eye to turn red.
The eye looks red when the blood vessels that are in the conjunctiva (the mucous membrane that covers the white of your eye and the backside of your eyelids) becomes dilated.
Those blood vessels often dilate when the eye gets irritated. This irritation can originate from a problem occurring inside the eye or factors from outside the eye.
The most common external factors that can cause the eye to become red are exposure to infectious organisms (mostly viruses and bacteria), environmental irritants (smoke, chemicals, sunlight), or allergens.
Infectious organisms can cause infectious conjunctivitis, or what is more commonly referred to as “pink eye.” This condition often presents with the eye being red and a mucous discharge being produced, often to such a degree that the eyelids are crusted over upon awaking in the morning. Infectious conjunctivitis can be extremely contagious and it is often advised that you severely limit your exposure to others while the problem is active. Infectious conjunctivitis caused by bacteria can be treated with antibiotic eye drops but viral conjunctivitis currently has no treatment and must run its course like the common cold.
Environmental irritants can make the eye look red for a short period of time during and immediately after exposure. The irritation is usually self-limited but may resolve more quickly with the use of over-the-counter lubricating drops or artificial tears. It is very important to understand exactly which irritant you were exposed to because there are some chemicals (acids and bases) that can cause extreme damage to the eye. So if you’re exposed to a caustic chemical you need to immediately rinse your eye out with water and seek emergency medical attention.
Allergens can cause allergic conjunctivitis, which can look very similar to pink eye but usually has significantly less mucous discharge and is usually accompanied by fairly severe itching. Allergic conjunctivitis is not contagious and can usually be treated with anti-allergy eye drops.
Infectious and allergic conjunctivitis can cause mild discomfort and itching but they rarely cause significant pain or loss of vision. A red eye with significant pain, especially when accompanied by severe light sensitivity and vision loss, often indicates more significant problems such as iritis, angle closure glaucoma or a corneal ulcer, all of which require immediate medical attention. If your eye is red and there is significant pain do not assume you have pink eye--see your eye doctor immediately!
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

A common in-office procedure is an eye injection for treatment of various eye conditions, such as wet macular degeneration, diabetic retinopathy, or vein occlusion.
It is normal to be anxious prior to your first eye injection but knowing what to expect may alleviate some anxiety.
Your eye will be numbed with topical anesthetic drops. Usually, a cotton-tipped applicator soaked in anesthetic will be held against the white part of the eye to numb it. Sometimes, a thick gel may also be used for numbing. Once the eye is numbed, it will then be cleaned and a small instrument will be used to hold the eye open. During the actual injection, some patients feel pressure while others may feel a quick sting. Each person will have a different experience and each injection will be different.
The medicine is injected into the white part of the eye. Sometimes a blood vessel may be encountered during the injection and you may notice a little redness on the outside of the eye. This is purely a cosmetic symptom and the redness will disappear within the next couple of days. Patients may also experience some mild irritation after the injection due to the drops that are placed in the eye. I usually recommend over-the-counter artificial tears to use after the injections. Usually, the eye should feel normal by the next day.
Another common symptom after an injection are floaters. These floaters usually appear as small bubbles in the lower half of your vision, but they will disappear in in a day or two.
There are no activity restrictions after the injection and no antibiotic drops are needed.
Things to watch for after the injection:
- If your eye gets painful or redness develops a couple of days after the injection, then you should call your doctor.
- If your vision declines or you notice increased or hundreds of floaters then you should call to be seen.
Otherwise, patients are usually initially seen once a month after they first start injections.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Red, itchy, swollen eyelids are often due to a condition called blepharitis. Blepharitis tends to be a chronic condition due to thick eyelid mucous gland production that sticks to the bases of the eyelashes. This adherent mucous can allow bacteria to overgrow and also attract and retain allergens. The standard treatment for blepharitis is doing warm compresses and cleaning off the eyelids with a mild baby shampoo and water solution.This treatment works for some people, but there are many more sufferers who have chronic irritation and relapses despite this treatment. If the warm compresses and eyelid scrubs are not quite keeping the condition under control, there are several other additional treatments that can be used to control the symptoms.One such treatment that your doctor might decide upon is an antibiotic/steroid combination drop or ointment. We usually use these for short periods of time to try to bring the condition under control. They are not good to use chronically because it can lead to resistant bacteria and the steroid component can cause other eye issues like cataracts and glaucoma. The treatment is very safe for short term use, but chronic use is usually not a good option.There are also antibiotic eyelid scrubs such as Avenova which can be prescribed and used on a more long-term basis.Oral Doxycycline can also be used longer in very low doses. Doxycycline is an antibiotic that when used to treat infections is generally prescribed in a dose of 100mg twice a day. For chronic blepharitis sufferers we generally use a much lower dose of around 50 mg a day. At that dose we are using the Doxycycline more to help thin out the mucous production from the eyelid glands than for its antibiotic properties.In summary, blepharitis can be a chronic issue that requires some persistent “maintenance” work to be done to keep it under control, and sometimes further intervention is needed for flare-ups.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

We all know that during pregnancy, a woman's body goes through a great deal of change hormonally and physiologically. But did you know her eyes change as well? Below are some of the most common effects pregnancy can have on the eye.
- Corneal changes. In some cases, pregnancy can cause the cornea, the front window of the eye, to change curvature and even swell, leading to shifts in glasses and contact lens prescriptions. In addition, changes in the chemistry of the tear film can lead to dry eyes and contact lens intolerance. It is for these reasons that it is generally not recommended to have any new contact lens fitting or new glasses prescription checks until several months postpartum. We want to get the most accurate measurements possible.
- Retinal changes. Many different conditions can affect the retina during pregnancy. If the pregnant woman has diabetes, diabetic eye disease can progress by 50%. In women with preeclampsia, a condition where blood pressure rises significantly, over 40% of women can show changes in the retinal blood vessels, and 25% to 50% complain of changes to their vision.
- Eye Pressure Fluctuation. Intraocular pressure (IOP) usually decreases during pregnancy. The exact mechanism causing this is unknown, but it is usually attributed to an increase of flow of intraocular fluid out of the eye. This is good news for pregnant women with glaucoma or high IOP. In fact, the drop in IOP is larger when you start with a high IOP compared to one in the normal range.
There are many more effects that pregnancy can have on the eye, but these are the most common. One other thing to keep in mind is that though the likelihood of any adverse effect is extremely low, we try not to use any diagnostic eye drops on pregnant patients during the eye exam. Unless there is a medical necessity to dilate the pupils or check IOP, it is a good rule of thumb to put off using drops until after the patient has given birth in order to protect the developing baby.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

More middle-aged and older adults are wearing soft contacts than ever.
And one of the biggest reasons they stop wearing contacts is the difficulty they face reading with their contacts after presbyopia begins to set in around the early 40’s.
Presbyopia is the diminished ability of the natural lens in our eyes to focus up on close objects. It begins with the occasional medicine bottle being a struggle to read and then over time more and more gets blurry. It can be very frustrating to stare at something up close and have it be blurry regardless of what you do.
So there are three basic choices a contact lens wearer can do to aid their reading while still wearing contact lenses.
Reading Glasses
Initially, the use of an over-the-counter reader or prescription reading glass for occasional use works well for people in the early stages of presbyopia. They are worn over distance contact lenses so there is little adjustment and vision is clear near and far. However, they need to be with you, not left in the car or at work, and oftentimes people end up just wearing readers all day since it is just that much clearer.
Monovision
This fitting technique can be used with any type of contact lens. The brand of lenses you are currently wearing can often be used to fit you with monovision. Your dominant eye is determined. Then the non-dominant eye prescription is adjusted to be good for reading distance. So once fitted, you have one eye for distance and the other for reading. Yes, it sounds really crazy, but it can actually work quite well. Your brain initially has to adjust to using each eye individually to obtain the sharpest vision, but once this is achieved, year-to-year adjustments can be made to the reading eye to allow comfortable distance and reading vision for many years.
Monovision fits are not always successful. Some people just cannot adjust to it regardless of motivation or desire. It seems to work best when someone has had some difficulty with reading and they are noticing more and more that they need their readers. At that point, they can appreciate the ability to read and their brain seems to adapt more readily. When I wear my contacts this is the option I have used for myself.
Multifocal Contacts
Another option is multifocal contact lenses. Most major manufacturers of soft contact lenses have some type of disposable multifocal lens available. They do not work like multifocal glasses. They use a technique called simultaneous viewing, in which you are actually looking through all the powers at once.
To visualize this, imagine a vinyl record with the label in the center and the various tracks extending outward. Most of the lenses are made with the strongest reading power located in the center where the label would be, then each ring further out gradually becomes weaker until you reach your full distance power. So essentially you are looking “around” the reading part for distance and through the center for reading. It works, sort of.
Multifocal lenses work better on younger patients, say 40-50 years old, for help with reading. There is no adaptation period to these lenses like monovision. What you see is what you get. But if you have any significant amount of astigmatism or if you wear a toric contact that corrects for astigmatism, multifocal lenses are not for you. And because the reading part is in the center of the lens, if you that central prescription strong, then you can blur the distance vision a lot--so oftentimes a multifocal lens wearer after age 50 faces the dilemma of either wearing reading glasses to boost their reading needs or changing to monovision.
Conclusion
In conclusion, while none of the options are perfect, they all may present some level of relief in your quest to continue to wear contacts into middle age, retirement, and beyond. But some options may better serve you at a certain point in your life or career than others. Talk to your eye doctor to see what choices are best for you.
Article contributed by Eugene Schoener O.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Recent Census Bureau data shows a population of approximately 70 million baby boomers (the generation born from 1946-1964). What does that have to do with low vision you may ask? Approximately 40 million people worldwide have some sort of blindness, and aging increases the incidence of macular degeneration and other vision impairment that qualifies them as “low vision” persons.
Low vision is a condition of the eye in which the vision falls below 20/70 in the better seeing eye. It impairs the recipients, rendering them unable to perform daily tasks that others take for granted. With this rising aging population, the awareness of low vision therapy, diagnosis, and treatments are more widely available.
Low vision treatment can help people recover from decreased visual function due to retinal disease, brain injury, neurological damage, and other causes.
It is not only the elderly population that is affected--approximately 20% of low vision patients are children under the age of 18. Childhood genetic disorders of the eye such as retinitis pigmentosa, albinism, Bests disease, ROP, rod/cone disorders, and glaucoma are among the causes of low vision in the pediatric population.
What can be done to help these millions?
There are eye care practitioners and therapists that specialize in low vision. They train patients to adjust their current lifestyles to make them more independent and utilize the current salvageable vision they do have. For example, if a person has lost their central vision due to macular degeneration, they can be trained to use their peripheral vision for many tasks.
Because patients with low vision cannot be functionally corrected with regular eye glasses, the use of telescopes, magnifiers, computer generated aids, training, biofeedback, and optical magnification devices are among some of the resources available to help. Occupational therapists also employ orientation and mobility assistance to help patients in their daily living skills.
There are many technologies that help to improve vision. One such technology is a bionic eye device that uses a pair of glasses with a camera that transmits video data to an implant in the back of that patients eye (the retina). This device uses technology similar to cochlear implants that stimulate auditory nerve signals to restore hearing. In the same way, visual impulses can be restored by stimulating neurons in the retina, brain, or optic nerve.
Maybe the Bionic Man TV series wasn’t too far out there and can someday be a reality............restoring vision to millions.
For more valuable information on low vision visit:
American Optometric Association AOA
American Occupational Therapy Association AOTA
American Academy of Ophthalmology AAO
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Age-related macular degeneration, often called ARMD or AMD, is the leading cause of vision loss among Americans 65 and older.
AMD causes damage to the macula, which is the central portion of the retina responsible for sharp central vision. AMD doesn't lead to complete blindness because peripheral vision is still intact, but the loss of central vision can interfere with simple everyday activities such as reading and driving, and it can be very debilitating.
Types of Macular Degeneration
There are two types of macular degeneration: Dry AMD and Wet AMD.
Dry (non-exudative) macular degeneration constitutes approximately 85-90% of all cases of AMD. Dry AMD results from thinning of the macula or the deposition of yellow pigment known as drusen in the macula. There may be gradual loss of central vision with dry AMD, but it is usually not as severe as wet AMD vision loss. However, dry AMD can slowly progress to late-stage geographic atrophy, which can cause severe vision loss.
Wet (exudative) macular degeneration makes up the remaining 10-15% of cases. Exudative or neovascular refers to the growth of new blood vessels in the macula, where they are not normally present. The wet form usually leads to more serious vision loss than the dry form.
AMD Risk factors
- Age is the biggest risk factor. Risk increases with age.
- Smoking. Research shows that smoking increases your risk.
- Family history. People with a family history of AMD are at higher risk.
- Race. AMD is more common in Caucasians than other races, but it exists in every ethnicity.
- Gender. AMD is more common in women than men.
Detection of AMD
There are several tests that are used to detect AMD.
A dilated eye exam can detect AMD. Once the eyes are dilated, the macula can be viewed by the ophthalmologist or optometrist. The presence of drusen and pigmentary changes can then be detected.
An Amsler Grid test uses pattern of straight lines that resemble a checkerboard. It can be used to monitor changes in vision. The onset of AMD can cause the lines on the grid to disappear or appear wavy and distorted.
Fluorescein Angiogram is a test performed in the office. A fluorescent dye is injected into the arm and then a series of pictures are taken as the dye passes through the circulatory system in the back of the eye.
Optical coherence tomography (OCT) is a test based on ultrasound. It is a painless study where high-resolution pictures are taken of the retina.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

What Is Intraoperative Aberrometry?
Yes, that is a mouthful, but the concept isn’t quite as hard as the name.
An Intraoperative Aberrometer is an instrument we can use in the operating room to help us determine the correct power of the implant we put in your eye during cataract surgery.
Cataract surgery is the removal of the cloudy natural lens of your eye and the insertion of a new artificial lens inside your eye called an intraocular lens (IOL).
The cloudy cataract that we are removing has focusing power (think of a lens in a camera) and when that lens is removed, we need to insert an artificial lens in its place to replace that focusing power. The amount of focusing power the new IOL needs has to match the shape and curvature of your eye.
To determine what power of lens we select to put in your eye, we need to measure the shape and curvature of your eye prior to surgery. Once we get those measurements, we can plug those numbers into several different formulas to try and get the most accurate prediction of what power lens you need.
Overall, those measurements and formulas are very good at accurately predicting what power lens you should have. There are, however, several eye types where those measurements and formulas are less accurate at predicting the proper power of the replacement lens.
Long Eyes: People who are very nearsighted usually have eyes that are much longer than average. This adds some difficulty with the accuracy of both the measurements and the formulas. There are special formulas for long eyes but even those are less accurate than formulas for normal length eyes.
Short Eyes: People who are significantly farsighted tend to have shorter-than-normal eyes. Basically, the same issues hold true for them as the ones for longer eyes noted above.
Eyes with previous refractive surgery (LASIK, PRK, RK): These surgeries all change the normal shape of the cornea. This makes the formulas we use on eyes that have had previous surgery not work as well when the normal shape of the cornea has been altered.
This is where intraoperative aberrometry comes in. The machine takes the measurements that we do before surgery and then remeasures the eye while you are on the operating room table after the cataract is removed and before the new implant is placed inside the eye. It then presents the surgeon with the power of the implant that the aberrometer thinks is the correct one. Unfortunately, the power that the aberrometer selects isn’t always exactly right, but with the combination of the pre-surgery measurements and the intra-surgery measurements the overall accuracy is significantly enhanced.
The intraoperative aberrometry is also very helpful in choosing the power of specialty lenses like multi-focal and toric lenses.
We would encourage you to consider adding intraoperative aberrometry to your cataract surgery procedure if you have either a long or short eye (usually manifested as a high prescription in your glasses) or if you have had any previous refractive surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
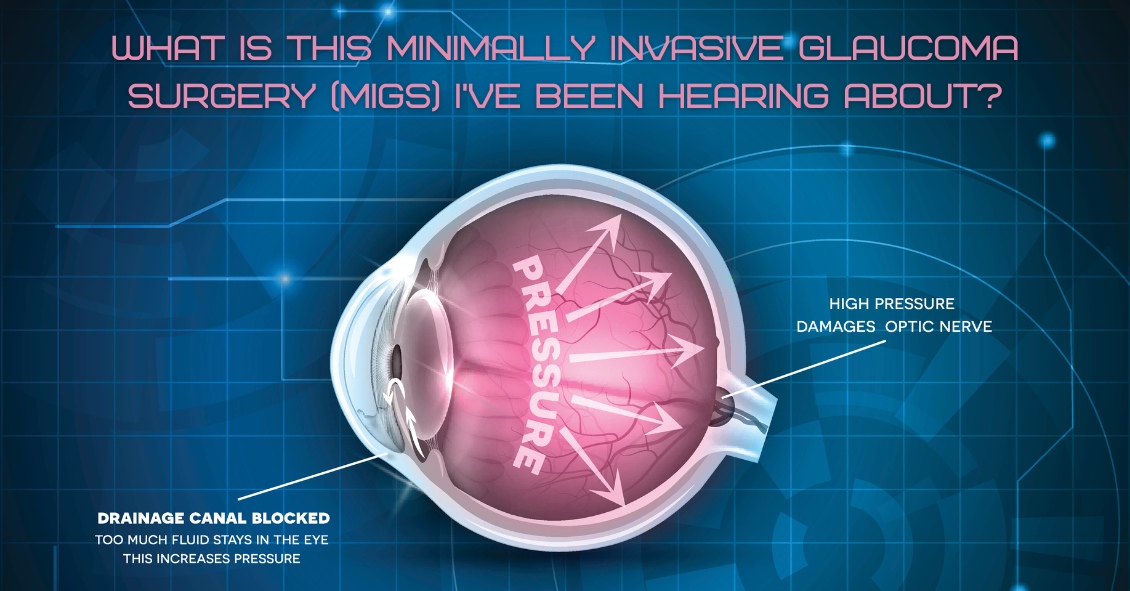
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the surgeon to intervene at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.

Is it safe to use "Redness Relief" eye drops regularly?
The short answer is NO.
Here’s the slightly longer answer.
There are several eye “Redness Relief” products on the over-the-counter market, such as those made by Visine, Clear Eyes, and Bausch & Lomb - as well as generic versions sold by pharmacy chains.
Most commonly, the active ingredient in redness relief drops is either Tetrahydrozoline or Naphazoline. Both of these drugs are in a category called sympathomimetics.
Sympathomimetics, the active ingredient in redness relief drops, work though a process called vasoconstriction, an artificial clamping down of the superficial blood vessels on the eye surface. These blood vessels often dilate in response to an irritation. This increase in blood flow is trying to help repair whatever irritation is affecting the surface of the eye. Clamping down on those vessels by using a vasoconstrictor counteracts the body’s efforts to repair the problem.
The other downside to repetitively using redness relief drops is that after the vasoconstrictor wears off the vessels often dilate to an even larger degree than when the process started. This stimulates you to use the drops again.
All of these drops carry these same two warnings on their labels:
Do not overuse as it may produce increased redness of the eye.
Stop using and ask a doctor if you experience eye pain, changes in vision, continued redness or irritation of the eye, condition worsens or persists for more than 72 hours.
Does anyone read those warnings? Almost never.
These drops are meant to be used for a VERY short duration - one or two days. That’s it!
They are not meant to be used indefinitely and they are certainly not meant to be used daily.
Take a good look at that first warning: MAY PRODUCE INCREASED REDNESS OF THE EYE.
If you are using redness relief drops repetitively you are likely making your eye redness WORSE, not better.
If you have been using redness relief drops daily you need to stop and replace them with an artificial tear or lubricating drop - something that DOES NOT say “gets the red out.”
After you make that switch your eyes are initially going to be red as your blood vessels take time to regain their normal vascular tone without the vasoconstrictor clamping down on them. The lubricating drop will actually help to repair the damage done by exposure to adverse conditions. This will decrease the inflammatory signals that make the vessels dilate. You will actually be doing something helpful to the surface of your eyes instead of just masking everything by artificially clamping down on your vessels and decreasing the flow of oxygen and nutrients to the front surface of your eye.
Using redness relief drops if you wear contacts is an even worse idea. If you put the drop in with your contact in, the contact will hold onto the drug and keep it on your eye surface longer, thus likely increasing the vasoconstriction.
Your cornea has no blood vessels in it and it depends on the blood vessels in the conjunctiva over the whites of the eye to bring in nutrients and oxygen. The other source of oxygen for the cornea is what it gets from diffusion from the atmosphere and that is also cut down by the presence of the contact lens.
The redness relief drop combined with the contact lens are now BOTH reducing the levels of oxygen getting to the cornea. Decreased oxygen to the cornea is one of the biggest risks for contact lens-related infections, including corneal ulcers.
Don’t get me wrong, I’m not condemning redness relief drops if used appropriately for a very short time to soothe the eyes if they have been temporarily exposed to elements that made them irritated. For a day or two redness relief drops are fine. But for long-term use or for use while wearing your contacts they are much more likely to cause problems than to provide any benefits.
Article contributed by Dr. Brian Wnorowski, M.D
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
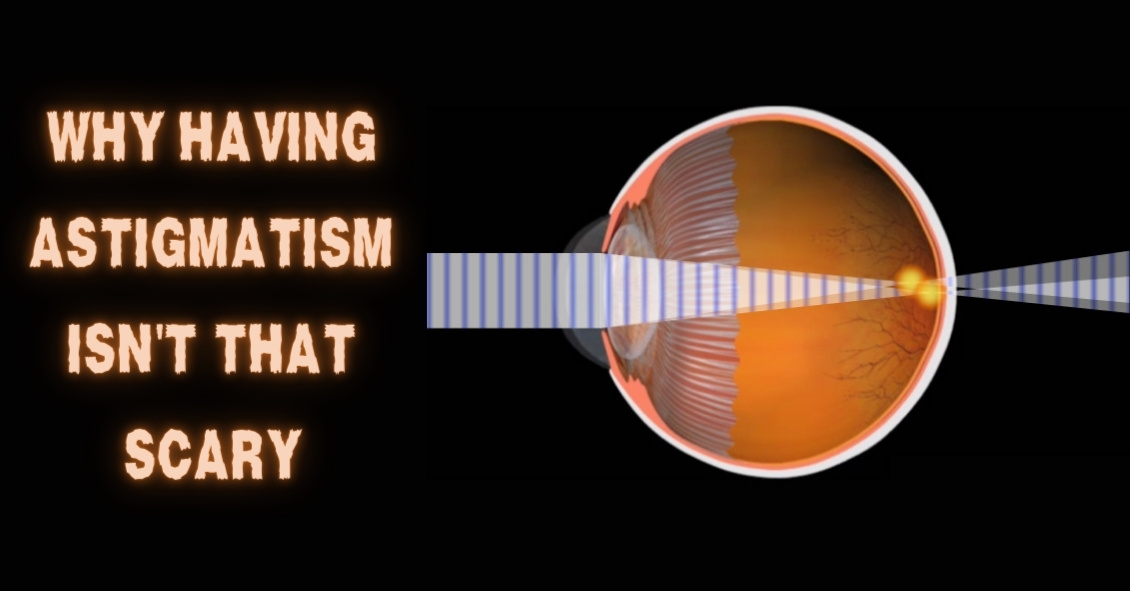
The word “astigmatism” is used so much in the optometric world that most people have talked about it when discussing their eye health with their doctor.
“Astigmatism” comes from the Greek “a” - meaning “without” - and “stigma” - meaning “a point.” In technical ocular terms, astigmatism means that instead of there being one point of focus in the eye, there are two. In other words, light merges not on a single point, but on two different points.
This is experienced in the real world as blurred, hazy vision, and can sometimes lead to eye strain or headaches if not corrected with either glasses or contact lenses.
Astigmatism is not a disease. In fact, more than 90% of people have some degree of astigmatism.
Astigmatism occurs when the cornea, the clear front surface of the eye like a watch crystal, is not perfectly round. The real-world example we often use to explain astigmatism is the difference between a basketball and a football.
If you cut a basketball in half you get a nice round half of a sphere. That is the shape of a cornea without astigmatism.
If you cut a football in half lengthwise you are left with a curved surface that is not perfectly round. It has a steeper curvature on one side and a flatter curve on the other side. This is an exaggerated example of what a cornea with astigmatism looks like.
The degree of astigmatism and the angle at which it occurs is very different from one person to the next. Therefore, two eyeglass prescriptions are rarely the same because there are an infinite number of shapes the eye can take.
Most astigmatism is “regular astigmatism,” where the two different curvatures to the eye lie 90 degrees apart from one another. Some eye diseases or surgeries of the eye can induce “irregular astigmatism,” where the curvatures are in several different places on the eye’s surface, and often the curvatures are vastly different, leading to a high amount of astigmatism.
Regular astigmatism is treated with glasses, contact lenses, or refractive surgery (PRK or LASIK). Irregular astigmatism, such as that caused by the eye disease keratoconus, usually cannot be treated with these conventional methods. In these circumstances, special contact lenses are needed to treat the condition.
The next time you hear that either you or a loved one has astigmatism, fear not.
It is easily corrected, and although astigmatism can cause your vision to be blurry, it rarely causes any permanent damage to the health of your eyes.
If you experience blurred vision, headaches, or eye strain, having a complete eye exam may lead to a diagnosis and treatment of this easily-dealt-with condition.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
There are several different variations of glaucoma, but in this article we will mainly focus on Primary Open Angle Glaucoma. This means that there is no specific underlying cause for the glaucoma, like inflammation, trauma or a severe cataract. It also means that the drainage angle where fluid is drained from the inside of the eye into the bloodstream is not narrow or closed.
Closed or Narrow Angle Glaucoma, which we won't be discussing today, is treated differently from Open Angle Glaucoma
In the U.S., Primary Open Angle Glaucoma (POAG) is by far the most common type of glaucoma we treat.
Glaucoma is a disease where the optic nerve in the back of the eye deteriorates over time, and that deterioration has a relationship to the Intraocular Pressure (IOP). Most - but not all - people diagnosed with glaucoma have an elevated IOP. Some people have fairly normal IOP’s but show the characteristic deterioration in the optic nerve. Regardless of whether or not the pressure was high initially, our primary treatment is to lower the IOP. We usually are looking to try to get the IOP down by about 25% from the pre-treatment levels.
The two mainstays of initial treatment for POAG in the U.S. are medications and laser treatments. There are other places in the world where glaucoma is initially treated with surgery. However, while surgery can often lower the pressure to a greater degree than either medications or laser treatments, it comes with a higher rate of complications. Most U.S. eye doctors elect to go with the more conservative approach and utilize either medications, most often in the form of eye drops, or a laser treatment.
Drops
There are several different classes of medications used to treat glaucoma.
The most common class used are the Prostaglandin Analogues or PGA’s. Some of the PGA’s available in the U.S. are Xalatan (latanaprost), Travatan (travapost), Lumigan (bimatoprost) and Zioptan (tafluprost).
PGA’s are most doctors’ first line of treatment because they generally lower the IOP better than the other classes, they are reasonably well tolerated by most people, and they are dosed just once a day. Most of the other drugs available have to be used multiple times a day.
The other classes of drugs include beta-blockers that are used once or twice a day; carbonic anhydrase inhibitors (CAI’s ), which come in either a drop or pill form and are used either twice or three times a day; alpha agonists that are used either twice or three times a day; and miotics, which are used three or four times a day. All of these other medications are typically used as either second-line or adjunctive treatment when the PGA’s are not successful in keeping the pressure down as single agents.
There are also several combination drops available in the U.S. that combine two of the second-line agents (Cosopt, Combigan, and Symbrinza).
Laser
The second option for initial treatment is a laser procedure.
Two common laser treatments for Open Angle Glaucoma are Argon Laser Trabeculoplasty (ALT) or Selective Laser Trabeculoplasty (SLT). These treatments try to get an area inside the eye called the trabecular meshwork - where fluid is drained from the inside of the eye into the venous system - to drain more efficiently.
These treatments tend to lower the pressure to about the same degree as the PGA’s do with over 80% of patients achieving a significant decrease in their eye pressure that lasts at least a year. Both laser treatments can be repeated if the pressure begins to rise again in the future, but the SLT works slightly better as a repeat procedure compared to the ALT.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Do you have family members with eye-related conditions?
The two main eye diseases in adults that have a genetic link are glaucoma and age-related macular degeneration (AMD).
Glaucoma is a deterioration of the optic nerve caused by pressure in the eye or poor blood flow to the optic nerve. It has no symptoms at its onset. In most cases if you wait to get glaucoma diagnosed until you begin to realize there is something wrong with your vision, upwards of 70% of your optic nerve will have already been destroyed. Once the nerve is destroyed there is no way of reversing that today and treatment is focused on trying to preserve whatever nerve tissue is left.
Your chances of getting glaucoma are four to 10 times higher if you have a close relative with glaucoma. Getting your eyes examined regularly is always important but even more so if there is a family history of glaucoma.
Macular degeneration is the leading cause of blindness in most of the developed world. It too can cause serious vision loss if you wait until you have significant symptoms before a diagnosis. There are now some preventative treatments for AMD--the earlier it is detected the better off you will be.
Having a close family member with AMD may increase your chances of having the disease as much as 50 percent, making timely diagnosis and treatment imperative.
Other eye diseases that run in families include strabismus (crossed eyes), myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
All of these family connections are important to know so that you and your eye doctor can together take the best possible care of your eyes. Before your next eye exam, ask your relatives if they have a history of eye disease. It might not make for the lightest of conversation at your next family gathering, but it could help save your vision.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Do you have family members with eye-related conditions?
The two main eye diseases in adults that have a genetic link are glaucoma and age-related macular degeneration (AMD).
Glaucoma is a deterioration of the optic nerve caused by pressure in the eye or poor blood flow to the optic nerve. It has no symptoms at its onset. In most cases if you wait to get glaucoma diagnosed until you begin to realize there is something wrong with your vision, upwards of 70% of your optic nerve will have already been destroyed. Once the nerve is destroyed there is no way of reversing that today and treatment is focused on trying to preserve whatever nerve tissue is left.
Your chances of getting glaucoma are four to 10 times higher if you have a close relative with glaucoma. Getting your eyes examined regularly is always important but even more so if there is a family history of glaucoma.
Macular degeneration is the leading cause of blindness in most of the developed world. It too can cause serious vision loss if you wait until you have significant symptoms before a diagnosis. There are now some preventative treatments for AMD--the earlier it is detected the better off you will be.
Having a close family member with AMD may increase your chances of having the disease as much as 50 percent, making timely diagnosis and treatment imperative.
Other eye diseases that run in families include strabismus (crossed eyes), myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
All of these family connections are important to know so that you and your eye doctor can together take the best possible care of your eyes. Before your next eye exam, ask your relatives if they have a history of eye disease. It might not make for the lightest of conversation at your next family gathering, but it could help save your vision.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Millions of people are affected by dry eye syndrome and the prevalence of dry eye increases with age. An estimated 3.2 million women and over and 1.68 million men age 50 and over are affected by dry eye syndrome.
Here are some risk factors for dry eye:
Aging: Advancing age is the single most important risk factor for dry eye. Most of our body’s moisture-producing glands produce less moisture as we age.
Gender: Women are twice as likely as men to suffer from dry eye. Changes in hormone levels throughout your lifetime often affect the amount of moisture produced by the lacrimal glands that produce tears.
Medical problems: Several diseases result in increased risk for dry eye syndrome, including rheumatoid arthritis, diabetes, thyroid abnormalities, asthma, cataracts, glaucoma, and lupus.
Medication: Certain medications can decrease the body's ability to produce lubricating tears.
Contact lenses: Dry eye is the leading cause of contact lens discomfort or intolerance.
Environmental conditions: Exposure to smoke, fluorescent lights, air pollution, wind, heat, air conditioning, and dry climates can increase tear evaporation.
Computer users: People who spend many hours staring at computer screens tend to blink significantly less often. Not blinking allows the eyes to dry faster.
Refractive surgery: This increases the risk of dry eye. Surgery often interferes with the superficial nerves on the cornea. Properly functioning nerves are necessary to help keep the eye surface moist.
Dry eye can present in many different ways. You can have irritation (often presenting as a foreign body feeling on the eye surface), redness, burning, excessive tearing (yes, that sounds counterintuitive but dry eye often presents this way), or intermittent blurring of vision.
The only way to be sure your symptoms are truly a dry eye problem is to have a comprehensive exam by your ophthalmologist or optometrist. There are other problems, such as allergic reactions and blepharitis, that can create similar symptoms so you need to be examined to determine which of these issues is causing your symptoms.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

In light of the holiday season, here are our top 10 eye care jokes.
1) What do you call a blind deer? No Eye Deer!
2) What do you call a blind deer with no legs? Still No Eye Deer!
3) Why do eye doctors live long lives? Because they dilate!
4) Why did the blind man fall into the well? He couldn’t see that well.
5) Why shouldn’t you put avocados on your eyes? Because you might get guac-coma!
6) What did the right eye say to the left eye? "Between you and me, something smells."
7) A man goes to his eye doctor and tells the receptionist he’s seeing spots. The receptionist asks if he’s ever seen a doctor. The man replies, “No, just spots.”
8) How many eye doctors does it take to screw in a light bulb? One … or two
9) Unbeknownst to her, a woman was kicked out of peripheral vision club. She didn’t see that one coming!
10) What do you call a blind dinosaur? A do-you-think-he-saurus
Bonus: What do you call a blind dinosaur’s dog? A do-you-think-he-saurus rex!
Article contributed by Dr. Jonathan Gerard

