Location & Hours
4008 Red Cedar Dr D-1
Highlands Ranch, CO 80126-8152
| Mon & Fri: | 8 - 4 |
| Tues - Thurs: | 10 - 7 |
No this is not a late-night personal injury lawyer infomercial.
This is a recommendation that you have your LASIK records available, for your own good, later in life.
There are 2 million cataract surgeries done yearly in the U.S. and the odds are, if you live long enough, you will eventually need cataract surgery, too.
What does this have to do with LASIK surgery?
When doctors perform cataract surgery they remove the cataract, which is the lens of your eye that has become cloudy. And they replace that lens with an artificial lens called an Intraocular Lens implant (IOL).
The IOL needs to have a strength to it to match your eye so that things are in focus without the need for strong prescription eyeglasses.
Currently, we determine what strength the IOL needs to be by using formulas that mostly depend on the measurements of the curvature of the cornea and the length of the eye.
Those formulas work best when the cornea is its natural shape -- i.e., not previously altered in shape from LASIK.
If you plug the “new” post-LASIK corneal shape into the formulas, the IOL strength that comes out is often significantly off the strength you really need to see well.
This is where having your records becomes important.
Knowing what your eyeglass prescription and corneal shape were BEFORE you had LASIK greatly improves our formula’s ability to predict the correct implant strength.
In most states there is a limit to how long a doctor needs to keep your records after your last visit, so everyone who has had LASIK surgery should get a copy of your pre- and post-LASIK records NOW before they no longer exist.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The Background
Over the last several years, research has indicated a strong correlation between the presence of Obstructive Sleep Apnea (OSA) and glaucoma. Information from some of these pivotal studies is presented below.
Did you know
- Glaucoma affects over 60 million people worldwide and almost 3 million people in the U.S.
- There are many people who have glaucoma but have not yet had it diagnosed.
- Glaucoma is a leading cause of blindness in the United States.
- If glaucoma is not detected and goes untreated, it can result in peripheral vision loss and irreversible blindness.
- Sleep apnea is a condition that obstructs breathing during sleep.
- It affects 100 million people around the globe and around 25 million people in the U.S.
- A blocked airway can cause loud snoring, gasping, or choking because breathing stops for up to two minutes.
- Poor sleep due to sleep apnea results in morning headaches and chronic daytime sleepiness.
The Studies
In January 2016, a meta-analysis by Liu et. al., reviewed studies that collectively encompassed 2,288,701 individuals over six studies. Review of the data showed that if an individual has OSA there is an increased risk of glaucoma that ranged anywhere from 21% to 450% depending on the study.
Later in 2016, a study by Shinmei et al. measured the intraocular pressure in subjects with OSA while they slept and had episodes of apnea. Somewhat surprisingly, they found that when the subjects were demonstrating apnea during sleep, their eye pressures were actually lower than when the events were not happening.
This does not mean there is no correlation between sleep apnea and glaucoma - it just means that an increase in intraocular pressure is not the causal reason for this link. It is much more likely that the correlation is caused by a decrease in the oxygenation level (which happens when you stop breathing) in and around the optic nerve.
In September of 2016, Chaitanya et al. produced an exhaustive review of all the studies done to date regarding a connection between obstructive sleep apnea and glaucoma and came to a similar conclusion. The risk for glaucoma in someone with sleep apnea could be as high as 10 times normal. They also concluded that the mechanism of that increased risk is most likely hypoxia – or oxygen deficiency - to the optic nerve.
A more recent study showed that even when factors such as age, gender, and disease are taken into account, there was up to a 40% greater chance of developing glaucoma when obstructive sleep apnea is present.
The Conclusion
There seems to be a definite correlation between having obstructive sleep apnea and a significantly increased risk of getting glaucoma. That risk could be as high as 10 times the normal rate.
It's highly recommended that if you have been diagnosed with obstructive sleep apnea that you have have a comprehensive eye exam in order to detect your potential risk for glaucoma.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

There are many options available to adults and children for corrective lenses (glasses and contacts) when engaged in physical activities.
Here is a look at the different modalities and the pros and cons of each:
Prescription Sports Goggles (e.g., Rec Specs)
The main benefits of goggles while playing sports are vision stability and eye protection. When playing fast-moving sports--like basketball, soccer, and rugby--elbows, wrists, and heads fly around at high speed, increasing the risk of eye injury. The eyes and eye sockets can be protected when covered by shatter-proof lenses. Additionally, there is no worry over having a contact lens pop out of the eye, which can be a debilitating experience for some people. The main drawback to goggles is that they can be cumbersome, decrease peripheral vision, and fog up. Additionally, very high prescriptions might not be available due to frame limitations. On the whole, this is a very good option for many people. One additional advantage to sports goggles is that they can often be made with Transitions lenses, providing automatic sun protection in bright light.
Contact Lenses
For many people, the best visual option is contact lenses, particularly soft contact lenses. The main benefits include no decrease in visual field, no fogging of lenses, and no unsightly, heavy glasses. But where sports goggles shine, contact lenses fall short--there is a higher risk of injury, the possibility of less stable vision (especially when wearing multifocal or astigmatic lenses), and the potential of a lens falling out during activities. Gas permeable (hard) lenses are not recommended for sports.
Wearing Nothing
For those whose prescriptions are not so high as to prevent proper functioning without correction, wearing no correction whatsoever is a fine choice. I’m often asked by parents whether their child absolutely needs to wear correction when they are playing sports. It really depends on how high the prescription is and the activity in which the child is engaged. If someone can see well enough to perform the goals without being hindered, not wearing any correction is perfectly fine.
There are plenty of options available for athletes. Visit your eye doctor to see what the best option is for your particular needs.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Hydroxychloroquine (Plaquenil) was originally used to treat malaria and is now commonly used to treat rheumatological and dermatological diseases. It is frequently used for rheumatoid arthritis (RA) and Lupus and is often very effective in mitigating the joint and arthritic symptoms these diseases can cause.
One of the most significant side effects of the drug is its possibility of causing eye problems resulting in blurred or decreased vision. The most common issue is damage to the retina. It can impair color vision or damage the retinal cells, particularly in the area right around the central vision.
In your retina, the area that you use to look straight at an object is called the fovea. The fovea is the area that provides you with the most definition when looking at an object. The area just around the fovea is called the macula and it has the ability to see objects with slightly less definition than the fovea but significantly better than the rest of your retina, which accounts for your peripheral vision. The most common place for hydroxychloroquine to cause a problem is in a ring of the macula surrounding the fovea.
The reason it is important to detect any of these changes as early as possible is because in many instances the changes are not reversible even if you come off the medication.
The risk of this happening is highly correlated with the cumulative dose of the drug you have received. So, the higher the dose and the longer you have been on it the higher your risk.
The current recommendation is a daily dose that does not exceed 6.5 mg/kg/day (that is milligrams per kilograms per day). There are approximately 2.2 pounds in a kilogram. The pills come in 200 mg tablets. Most people who are on this drug are on either 200 mg once a day or 200 mg twice a day. The safety break point comes at around 135 pounds. People weighing more than that will stay within the safety guidelines (not more than 6.5mg/kg/day) at 400mg per day, but people under 135 pounds should probably only be taking 200 mg per day.
Other risk factors for hydroxychloroquine retinal toxicity include kidney or liver disease and obesity. Obesity is a risk factor because the drug does not penetrate fat tissue so there is more of the drug in your lean body mass (including your retina and its supporting cells called the retinal pigment epithelium). What that means in real terms is that if you take two people who each weigh 140 pounds and put them both on 400 mg a day and one person is 4-foot 11 and the other is 5-foot 9, the 4-foot 11 inch person is at greater risk for side effects because the shorter person has more of their body weight in fat tissue. Since the hydroxychloroquine can’t penetrate the fat tissue, there is a higher concentration of it in sensitive tissues like the retina. People with kidney and liver problems have a tougher time eliminating the drug from their system so they are at higher risk because the body is going to retain more of the drug for a longer period of time.
The recommendation is to have a baseline eye exam with dilation and a visual field test before or soon after starting the drug. A repeat of that exam should occur every year if there is no evidence of toxicity.
The actual incidence of retinal toxicity from hydroxychloroquine is difficult to pin down because there is usually a long time between being started on the drug and the start of any identifiable retinal toxicity. The overall rate of probable retinal toxicity is in the range of 1 of every 200 people treated. The rate is much lower than that in the first 7 years of treatment but gets to about 5 times higher after 7 years of treatment. Some of that data is old now and there is much greater awareness currently about keeping people below that 6.5 mg/kg/day dosage level.
I have been in practice for over 25 years and have seen “probable” retinal toxicity from hydroxychloroquine a total of 5 times and only once in the last 10 years--when people have been more careful about keeping the dosage in the right range.
The drug can be very effective in its treatment of RA and Lupus and the likelihood of serious vision problems is small and can potentially be avoided with the correct dosing and monitoring of the eyes. Other drugs in the treatment for RA or lupus may have more frequent or serious side effects then hydroxychloroquine--so it would be wise to consider it a viable treatment option and not easily dismiss it because of the risk of what amounts to a fairly infrequent eye issue.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The Centers for Disease Control estimates that around 2.8 million people in the United States suffer from a traumatic brain injury (TBI) every year, and vision can be affected. Concussions are a type of TBI.
The rate of childhood TBI visits to the emergency department more than doubled between 2001 and 2009, making children more likely than any other group to go to the ER with concussion symptoms.
It was once assumed that the hallmark of a concussion was a loss of consciousness. More recent evidence, however, does not support that. In fact, the majority of people diagnosed with a concussion do not experience any loss of consciousness. The most common immediate symptoms are amnesia and confusion.
There also are multiple visual symptoms that can occur with a concussion, either initially or during the recovery phase.
Visual symptoms after a concussion include:
Blurred vision.
Difficulty reading.
Double vision.
Light sensitivity.
Headaches accompanying visual tasks.
Loss of peripheral vision.
Most people with visual complaints after a concussion have 20/20 distance visual acuity, so more specific testing of near acuity, convergence amplitudes, ocular motility, and peripheral vision must be done.
In a study done at the Minds Matter Concussion Program at the Children's Hospital of Philadelphia, patients with a concussion diagnosis underwent extensive vision testing, which assessed symptoms, visual acuity, eye alignment, near point of convergence, vergence amplitude and facility, accommodative amplitude and facility, and saccadic eye movement speed and accuracy.
A total of 72 children (mean age 14.6 years) were examined, and 49 (68%) of those were found to have one or more vision symptoms after concussion. The most common problems were convergence insufficiency (47.2%); accommodative insufficiency (33.3%); saccadic dysfunction (30.5%); and accommodative infacility (11.1%). The investigators also found that 64% of the children with convergence insufficiency also had an accommodative disorder.
Difficulties with accommodation and convergence make it very hard to read for any length of time, with blurring and fatigue and then loss of concentration occurring after a fairly short period of reading time.
For the majority of people suffering a mild to moderate TBI, most of these symptoms resolve in one to three weeks but in some they can persist much longer.
If your visual symptoms after a concussion persist past three weeks, a visit with an eye care specialist is recommended. There may be several options to help improve the symptoms with either prescription eyeglasses or prisms to assist the two eyes to focus together.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The majority of cataract surgeries performed in the U.S. are done with a local anesthetic and IV sedation.
The local anesthesia may be accomplished in one of two ways: either an injection of anesthetic around the eye or anesthetic eye drops placed on the eye, often combined with an injection of a small amount of anesthetic into the front of the eye at the very beginning of surgery.
The injection of anesthetic around the eye generally produces a deeper anesthesia for the surgery than the topical method but it also comes with increased risk. There is a very small chance of potentially serious bleeding behind the eye and a rare chance of inadvertent penetration of the back of the eye with the injection needle.
The topical anesthesia has lower risk but does not provide quite as much numbing, although the overwhelming majority of people having cataract surgery with a topical anesthetic do not experience any significant pain during the procedure.
The other difference between the two types of anesthesia is that with topical anesthesia you maintain your ability to move your eye around, whereas with injection anesthesia, the eye muscles are temporarily paralyzed so your eye doesn’t move during the surgery. When you have topical anesthesia it is important for you to try to stare straight ahead at the light in the microscope above you. Most people accomplish this quite easily.
Along with the anesthetic to the eye, an anesthetist will usually also give you some mild sedative medication through an IV. This relaxes you but does not put you “out,” although some people do fall asleep during the procedure from the effects of the sedation.
Many people who have cataract surgery with IV sedation don’t remember some of the surgery because of the amnesiac effect that occurs from the sedative. This often doesn’t happen when you return for surgery on your second eye.
Despite often getting the exact same dose of sedative on the second surgery, you have significant less amnesia the second time. This is caused by a quick buildup in tolerance to the medication.
When they have their second surgeries, many patients feel that the surgery was significantly different than the first time even though it was done exactly the same. The reason is just that you remember more the second time.
On rare occasions people need to have general anesthesia to have their cataracts removed. Today, that is mostly done for people who are incapable of cooperating and staying still for the surgery. For everyone who can cooperate, it is generally not worth the risks, which include death, to put people to sleep for a surgery that is easily done under a local anesthetic.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

In honor of St. Patrick’s Day and the “wearin’ of the green,” we thought it would be fun and fitting to share some interesting facts about green…eyes!
#1
Green is the rarest eye color. If your sparklers are truly green, you are something of a unicorn… only about 2% of the world’s population sport this hue.
#2
Green-eyed people can be found all around the globe. There is a Chinese village, Liqian, where a high percentage of the population sports green eyes and lighter hair.
#3
There isn’t any actual green pigment in a green eye. Melanin, a natural pigment that helps determine our skin, hair, and eye color, is found in all eyes. Brown eyes have quite a lot and blue eyes have relatively little. Green eyes are also low on melanin, but in addition they contain lipochrome, a yellowish, fat-soluble pigment. Lipochrome is also found in things like butter, eggs, and corn. So a little melanin, some lipochrome, and a cool light dispersing scattering called the Tyndall Effect combine to produce those rare green eyes!
#4
At least 16 genes contribute to eye color. You might have been taught in biology class that two brown-eyed parents can have only brown-eyed children, but it’s more complicated than that.
#5
Green eyes are popular in cultural references. Here are some famous characters with green eyes:
· Jane Eyre—that plucky governess living in a “haunted” mansion, from the book Jane Eyre
· Rapunzel—another courageous hero in Tangled
· Scarlet O’Hara—feisty protagonist in Gone with the Wind
· Scar—the scheming uncle in The Lion King
· Mary Jane Watson, Catwoman, Batgirl—green eyes are popular in the world of comics
· Sara Crewe—brave little girl from A Little Princess
· Harry Potter – from the Harry Potter book series by J.K. Rowling
#6
In a large survey performed by All About Vision, green was voted the most attractive eye color, with over 20% of the 66,000 respondents choosing this hue.
#7
More women than men have green eyes. Scientists aren’t sure why this is, but it suggests there is an underlying gender-related factor that causes this difference.
#8
 Animals can also sport green eyes. Green eyes occur in dogs, snakes, frogs, birds, monkeys, multiple members of the cat family, and many other animals.
Animals can also sport green eyes. Green eyes occur in dogs, snakes, frogs, birds, monkeys, multiple members of the cat family, and many other animals.
#9
People with green eyes are more likely to have certain health issues. Green eyes are more prone to melanoma of the uvea, a type of eye cancer, than are dark eyes. The same is true for macular degeneration. If you have green eyes, protect those beautiful peepers with a quality pair of sunglasses to lower your chances for these diseases!

A common question asked during the eye exam is, “When is the puff coming?”
Patients are referring to air-puff or non-contact tonometry. Tonometry is the procedure used to measure eye pressure, and this is important for diagnosing and monitoring glaucoma.
In non-contact tonometry, a puff of air is used to measure the pressure inside the eye. The benefit of this test is there is no actual contact with the eye, but the air puff is sometimes very startling for patients. Some people hate that test and it isn’t the most accurate way to measure your eye pressure.
Some doctors don’t even use the air-puff test. Instead, they place a yellow drop that consists of a numbing medicine and then shine a blue light on the eye. This is done in front of the slit lamp and a small tip gently touches the eye to measure the eye pressure. This procedure is called Goldmann tonometry and is considered the gold standard for measuring eye pressure.
Another method for checking eye pressure is the Tonopen. This is a portable, hand-held instrument that is useful when patients can’t sit in front of the slit lamp to have their eye pressure checked. The Tonopen also requires a numbing drop to be placed in the eye, and the tip gently touches the eye.
A common question related to tonometry is “what normal eye pressure?”
Normal eye pressure ranges from 10-21 mm Hg. Eye pressure doesn't have any relationship to blood pressure. Many times, people are surprised that their eye pressure is high, but they have normal blood pressure. In general, there is no diet or exercise that will significantly affect eye pressure. It is therefore important to have your eye pressure checked regularly because there are usually no symptoms of high eye pressure until it has affected your vision.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Have you ever seen a temporary black spot in your vision? How about jagged white lines? Something that looks like heat waves shimmering in your peripheral vision?
If you have, you may have been experiencing what is known as an ocular migraine. Ocular migraines occur when blood vessels spasm in the visual center of the brain (the occipital lobe) or the retina.
These optical migraines can take on several different symptoms, but they typically last only from a few minutes to an hour. They can take on either positive or negative visual symptoms, meaning they can produce what looks like a black blocked-out area in your vision (negative symptom), or they can produce visual symptoms that you see but know aren’t really there, like heat waves or jagged white lines that look almost like lightning streaks (positive symptoms).
Some people do get a headache after the visual symptoms but most do not. They get the visual symptoms, which resolve on their own in under an hour, and then generally just feel slightly out of sorts after the episode but don’t get a significant headache. The majority of episodes last about 20 minutes but can go on for an hour. The hallmark of this problem is that once the visual phenomenon resolves the vision returns completely back to normal with no residual change or defect.
If you have this happen for the first time it can be scary and it is a good idea to have a thorough eye exam by your eye doctor soon after the episode to be sure there is nothing else causing the problem.
Many people who get ocular migraines tend to have them occur in clusters. They can have three or four episodes within a week and then may not have another one for several months or even years.
There are some characteristics that raise your risk for ocular migraines. The biggest one is a personal history of having migraine headaches. Having a family history of migraines also raises your risk, as does a history of motion sickness.
Although the symptoms can cause a great deal of anxiety, especially on the first occurrence, ocular migraines rarely cause any long-term problems and almost never require treatment as long as they are not accompanied by significant headaches.
So if symptoms like this suddenly occur in your vision, try to remain calm, pull over if you are driving, and wait for them to go away. If they persist for longer than an hour, you should seek immediate medical attention.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Eye doctors typically pride themselves on being able to improve someone’s vision through glasses or contact lens prescriptions. Whether it’s a first-time glasses wearer, or someone having either a small or large change in their prescription, we like to aim for that goal of 20/20 vision.
Despite our best efforts, however, correcting vision to 20/20 is not always a positive outcome for the patient. Whether someone will be able to tolerate their new prescription is based on something called neuroplasticity, which is what allows our brains to adapt to changes in our vision.
You or someone you know may have had this happen: Your vision was blurry, so you went to the eye doctor. The doctor gave you a new prescription, but after you received your new glasses, things seem “off.”
Common complaints are that the prescription feels too strong (or even too clear!) or that the wearer feels dizzy or faint. This is especially true with older patients who have had large changes in their prescriptions, since neuroplasticity decreases with age. It is also more likely to happen when the new prescription has a change in the strength or the angle of astigmatism correction. Conversely, this happens less often in children, since their brains have a high amount of plasticity.
Quite often, giving the brain enough time to adapt to the new vision will decrease these symptoms.
Whenever a patient has a large change in prescription, I tell them that they should wear the glasses full time for at least one week. This is true for both large changes in prescription strength, as well as changing lens modality, e.g., single vision to progressives.
Despite the patient’s best efforts, though, sometimes allowing time to adapt to the new vision isn’t enough, and the prescription needs to be adjusted. Even when someone sees 20/20 on the eye chart with their new glasses, if they are uncomfortable in them even after trying to adjust for a week then we sometimes have to make a compromise and move the script back closer to their previous script so that there is less change and they can more easily adapt.
In conclusion, adapting to a new prescription can sometimes be frustrating. It does not mean there is anything wrong with you if you have difficulty adjusting to large changes in a prescription. With a little patience and understanding about how your brain adapts to these kinds of changes, your likelihood of success will be that much higher.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the surgeon to intervene at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.
Age-related macular degeneration, often called ARMD or AMD, is the leading cause of vision loss among Americans 65 and older.
AMD causes damage to the macula, which is the central portion of the retina responsible for sharp central vision. AMD doesn't lead to complete blindness because peripheral vision is still intact, but the loss of central vision can interfere with simple everyday activities such as reading and driving, and it can be debilitating.
Types of Macular Degeneration
There are two types of macular degeneration: Dry AMD and Wet AMD.
Dry (non-exudative) macular degeneration constitutes approximately 85-90% of all cases of AMD. Dry AMD results from thinning of the macula or the deposition of yellow pigment known as drusen in the macula. There may be gradual loss of central vision with dry AMD, but it is usually not as severe as wet AMD vision loss. However, dry AMD can slowly progress to late-stage geographic atrophy, which can cause severe vision loss.
Wet (exudative) macular degeneration makes up the remaining 10-15% of cases. Exudative or neovascular refers to the growth of new blood vessels in the macula, where they are not normally present. The wet form usually leads to more serious vision loss than the dry form.
AMD Risk factors
- Age is the biggest risk factor. Risk increases with age.
- Smoking. Research shows that smoking increases your risk.
- Family history. People with a family history of AMD are at higher risk.
- Race. AMD is more common in Caucasians than other races, but it exists in every ethnicity.
- Light eyes. Blue and hazel eyes are more prone to AMD than brown eyes.
- Gender. AMD is more common in women than men.
- High blood pressure.
- Diet high in saturated fat.
Detection of AMD
There are several tests that are used to detect AMD.
A dilated eye exam can detect AMD. Once the eyes are dilated, the macula can be viewed by the ophthalmologist or optometrist. The presence of drusen and pigmentary changes can then be detected.
An Amsler Grid test uses pattern of straight lines that resemble a checkerboard. It can be used to monitor changes in vision. The onset of AMD can cause the lines on the grid to disappear or appear wavy and distorted.
Fluorescein Angiogram is a test performed in the office. A fluorescent dye is injected into the arm and then a series of pictures are taken as the dye passes through the circulatory system in the back of the eye.
Optical coherence tomography (OCT) is a test based on ultrasound. It is a painless study where high-resolution pictures are taken of the retina.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
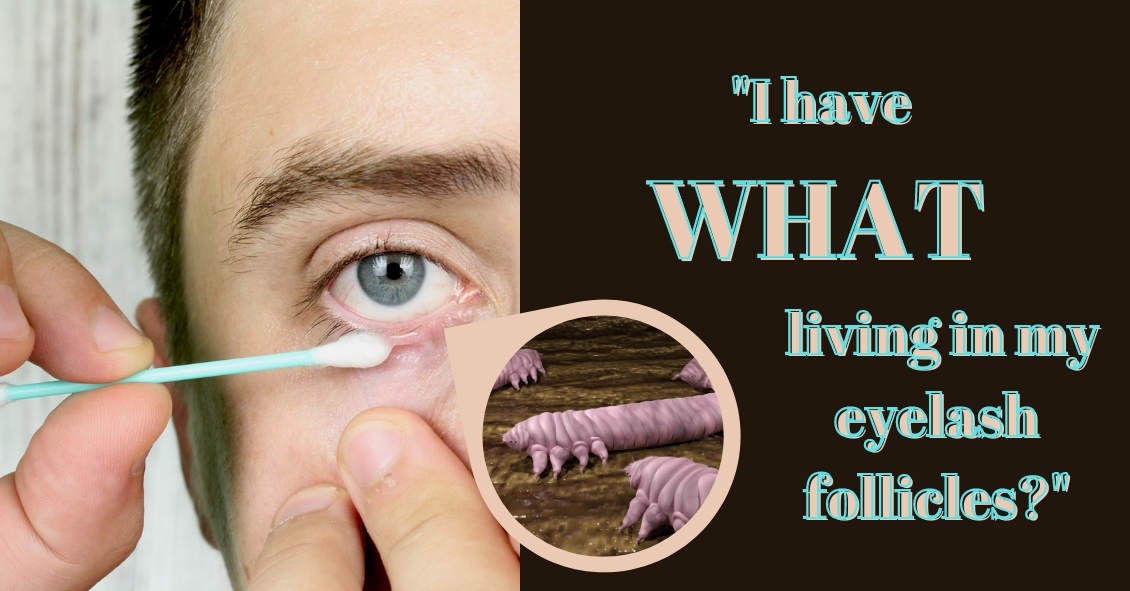
Demodex folliculorum -- often just called demodex -- is a mite that occurs naturally on many people's faces and resides in hair follicles, particularly the follicles of eyelashes. Most of the time, these mites cause no problems whatsoever. However, sometimes an infestation can become particularly parasitic, resulting in unhealthy eyelid margins. This inflammation of the eyelid is called blepharitis. Blepharitis can be caused by caused by several things, including allergies, bacterial overgrowth, Rosacea and also by demodex.
Often, diagnosis of mite infestation by your eye doctor can be difficult. The symptoms can mimic other causes of blepharitis, which is one of the most prevalent diseases we see.
The most common sign of a demodex infestation is a cylindrical cuff or "sleeve" at the base of the eyelash. Symptoms include redness, itching, burning, dry eyes and general discomfort in the eyelid.
The probability of demodex infestation increases gradually with age, with nearly 100% of people having demodex in their eyelashes after age 70. If there are no symptoms present, nothing needs to be done about demodex, as they are a natural occurrence. If any of the before-mentioned symptoms are present, however, eyelid hygiene using tea tree oil is often the first line treatment. Tea tree oil is known to kill the mites and there are now several brands of “eye lid scrubs” that come with tea tree oil in them.
There are also often in-office methods available for exfoliating eyelids.
If you're experiencing any demodex symptoms, make an appointment to see what treatment might be right for you.
Article contributed by Dr. Jonathan Gerard, O.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

There are many opinions on the topic of texting and driving. The goal of this blog post is to explore the effects on vision during texting.
So, from a visual perspective, why does texting make you more likely to crash? The problem lies in distraction from driving. For example, it takes a fast texter approximately 20 seconds to read and reply to a text. At 55 mph on the highway, a driver glances away from the road for approximately one-third of a mile. When the driver is focusing on their screen, this essentially gives the driver tunnel vision, causing the visual system to essentially use peripheral vision for driving. Your central vision is used to detect depth perception, detail, and colors such as red or green. So when texting, your depth perception, or 3-D vision, is altered and if cars are stopped ahead or closing in rapidly, it's not as easily detected. Colors, such as red brake lights or traffic signals, are not as easily noticed.
Next time you encounter situations with texting and driving, know that the visual system was designed to perform advanced visual perception while using central vision. This includes detail vision, depth perception, and color vision....all of which are placed on hold while texting and driving.
For more information on texting and driving see:
US Dept. of Transportation
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

We commonly see patients who come in saying that their eyes are bleeding.
The patient is usually referring to the white part of their eye, which has turned bright red. The conjunctiva is the outermost layer of the eye and contains very fine blood vessels. If one of these blood vessels breaks, then the blood spreads out underneath the conjunctiva. This is called a subconjunctival hemorrhage.
A subconjunctival hemorrhage doesn't cause any eye pain or affect your vision in any way. Most of the time, a subconjunctival hemorrhage is asymptomatic. It is only noticed when looking at the mirror or when someone else notices the redness of the eye. There should not be any discharge or crusting of your lashes. If any of these symptoms are present, then you may have another eye condition that may need treatment.
What causes a subconjunctival hemorrhage? The most common cause is a spontaneous rupture of a blood vessel. Sometimes vigorous coughing, sneezing, or bearing down can break a blood vessel. Eye trauma and eye surgery are other causes of subconjunctival hemorrhage. Aspirin and anticoagulant medication may make patients more susceptible to a subconjunctival hemorrhage, but there is usually no need to stop these medications.
There is no treatment needed for subconjunctival hemorrhage. Sometimes there may be mild irritation and artificial tears can be used. The redness usually increases in size in the first 24 hours and then will slowly get smaller and fade in color. It often takes one to two weeks for the subconjunctival hemorrhage to be absorbed. The larger the size of the hemorrhage, the longer it takes for it to fade.
Having a subconjunctival hemorrhage may be scary initially but it will get better in a couple of weeks without any treatment. However, redness in the eye can have other causes, and you should call your eye doctor, particularly if you have discharge from the eye.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Do you have floaters in your vision?
Floaters are caused by thick areas in the gel-like fluid that fills the back cavity of your eye, called the vitreous.
Many people, especially highly near-sighted people, often see some number of floaters for a good portion of their lives. Often, these floaters are in the periphery of the vision and may only be visible in certain lighting conditions. The most frequent conditions are when in bright sunlight looking toward the clear blue sky. I know this from personal experience since I have a floater in my left eye that I most often see when swimming outdoors. Every time I turn my head to the left to breathe I see this floater moving in my peripheral vision.
This is totally harmless other than when I’m swimming in the ocean and swear that sudden object in my peripheral vision is a shark bearing down on me. Some people who have floaters are not as lucky-- the floater might be in their central vision and is almost constantly annoying, especially when trying to read.
The second scenario in which floaters occur is during the normal aging process. The vitreous gel in the back of the eye starts to shrink as we age and at some point it collapses in on itself and pulls away from the retina. This sometimes results in a sudden set of new floaters.
When that happens you need to be checked for signs of a retinal tear or detachment. As long as your retina survives that episode without any problems, the floaters themselves may stick around for a while and can be rather annoying.
Most people eventually adapt to the floaters; the brain learns to filter them out so they are no longer aware of them. The vitreous can also collapse more as time goes on and the dense floater can initially may move further forward and drop lower in the eye so the shadow it is casting is less intense and more in the periphery of your vision where it is much easier to ignore.
The first line of treatment for floaters has been, and still is, to learn to live with them. Once you have your retina checked and verify that there is nothing wrong there, the floaters themselves are harmless and will not lead to any further deterioration of your vision--which is why, if at all possible, you should just live with them. This is especially true if the floaters are new because the overwhelming majority of people with new floaters will eventually get to the point where they are no longer seeing them or at least where they are not interfering with normal daily activities.
If you have tried to wait them out and live with them but they are still interfering with your normal daily activities, you may want to consider having them treated with a laser.
This treatment involves using a special laser to try to break down large floaters into much smaller pieces that may no longer be visible. In a study of the laser treatment involving 52 patients, 36 were treated with the laser (a single laser treatment session) and 16 people had a sham treatment (meaning they went through everything the treated group did but did not actually have the real treatment done). In the people who were actually treated, 54% reported a significant improvement in the floater symptoms while 0% in the sham group reported any improvement (no placebo effect). There were no significant side effects in either group.
Some points to note in the above study:
54% of people treated noted a significant improvement in their floater symptoms with a single treatment. That’s clearly not anywhere near a guaranteed improvement.
Other people have noted an improvement after more than one session, bringing the total expected improvement into the 70% range, with one or more treatments.
Another point to note is that there were no significant side effects to the treatment.
Although true in this small study, it does not mean that there are no risks to the laser treatment. Although rare, there have been reports of damage to the retina, optic nerve, or the lens of the eye.
Another treatment that can be used to treat floaters is a surgical procedure called a vitrectomy. This involves surgically going inside the back of the eye and removing the vitreous. This surgical procedure carries a higher risk than the laser treatment and is not 100% effective.
In summary, laser treatment is a good addition to the tools to deal with significant floater problems. If you have floaters for at least six months and they are in your central vision and interfering with your normal daily activities and you want to see if this laser treatment could be right for you, check with your eye doctor.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

A common question asked during the eye exam is, “When is the puff coming?”
Patients are referring to air-puff or non-contact tonometry. Tonometry is the procedure used to measure eye pressure, and this is important for diagnosing and monitoring glaucoma.
In non-contact tonometry, a puff of air is used to measure the pressure inside the eye. The benefit of this test is there is no actual contact with the eye, but the air puff is sometimes very startling for patients. Some people hate that test and it isn’t the most accurate way to measure your eye pressure.
Some doctors don’t even use the air-puff test. Instead, they place a yellow drop that consists of a numbing medicine and then shine a blue light on the eye. This is done in front of the slit lamp and a small tip gently touches the eye to measure the eye pressure. This procedure is called Goldmann tonometry and is considered the gold standard for measuring eye pressure.
Another method for checking eye pressure is the Tonopen. This is a portable, hand-held instrument that is useful when patients can’t sit in front of the slit lamp to have their eye pressure checked. The Tonopen also requires a numbing drop to be placed in the eye, and the tip gently touches the eye.
A common question related to tonometry is “what is normal eye pressure?”
Normal eye pressure ranges from 10-21 mm Hg. Eye pressure doesn't have any relationship to blood pressure. Many times, people are surprised that their eye pressure is high, but they have normal blood pressure. In general, there is no diet or exercise that will significantly affect eye pressure. It is therefore important to have your eye pressure checked regularly because there are usually no symptoms of high eye pressure until it has affected your vision.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
We commonly see patients who come in saying that their eyes are bleeding.
The patient is usually referring to the white part of their eye, which has turned bright red. The conjunctiva is the outermost layer of the eye and contains very fine blood vessels. If one of these blood vessels breaks, then the blood spreads out underneath the conjunctiva. This is called a subconjunctival hemorrhage.
A subconjunctival hemorrhage doesn't cause any eye pain or affect your vision in any way. Most of the time, a subconjunctival hemorrhage is asymptomatic. It is only noticed when looking at the mirror or when someone else notices the redness of the eye. There should not be any discharge or crusting of your lashes. If any of these symptoms are present, then you might have another eye condition that could need treatment.
What causes a subconjunctival hemorrhage? The most common cause is a spontaneous rupture of a blood vessel. Sometimes vigorous coughing, sneezing, or bearing down can break a blood vessel. Eye trauma and eye surgery are other causes of subconjunctival hemorrhage. Aspirin and anticoagulant medication may make patients more susceptible to a subconjunctival hemorrhage but there is usually no need to stop these medications.
There is no treatment needed for subconjunctival hemorrhage. Sometimes there may be mild irritation and artificial tears can be used. The redness usually increases in size during the first 24 hours and then slowly decreases and fades. It often takes one to two weeks for the subconjunctival hemorrhage to be absorbed. The larger the size of the hemorrhage, the longer it takes for it to fade.
Having a subconjunctival hemorrhage may be scary initially, but it will get better in a couple of weeks without any treatment. However, redness in the eye can have other causes, and you should call your eye doctor--particularly if you have discharge from the eye.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Diabetic retinopathy is an eye condition that can affect the retina of people who have diabetes.
The retina is the light-sensitive tissue that lines the back of the eye, and it detects light that is then processed as an image by the brain. Chronically high blood sugar or large fluctuations in blood sugar can damage the blood vessels in the retina. This can result in bleeding in the retina or leakage of fluid.
Diabetic retinopathy can be divided into non-proliferative or proliferative diabetic retinopathy.
Non-proliferative diabetic retinopathy: In the early stage of the disease, there is weakening of the blood vessels in the retina that causes out-pouching called microaneurysms. These microaneurysms can leak fluid into the retina. There can also be yellow deposits called hard exudates present in the retina from leaky vessels.
Diabetic macula edema is when the fluid leaks into the region of the retina called the macula. The macula is important for sharp, central vision needed for reading and driving. The accumulation of fluid in the macula causes blurry vision.
Proliferative diabetic retinopathy: As diabetic retinopathy progresses, new blood vessels grow on the surface of the retina. These blood vessels are fragile, which makes them likely to bleed into the vitreous, which is the clear gel that fills the middle of the eye. Bleeding inside the eye is seen as floaters or spots. Over time, scar tissue can then form on the surface of the retina and contract, leading to a retinal detachment. This is similar to wallpaper contracting and peeling away from the wall. If left untreated, retinal detachment can lead to loss of vision.
Symptoms of diabetic retinopathy:
- Asymptomatic: In the early stages of mild non-proliferative diabetic retinopathy, the person will usually have no visual complaints. Therefore, it is important for people with diabetes to have a comprehensive dilated exam by their eye doctor once a year.
- Floaters: This is usually from bleeding into the vitreous cavity from proliferative diabetic retinopathy.
- Blurred vision: This can be the result of fluid leaking into the retina, causing diabetic macular edema.
Risk factors for diabetic retinopathy:
- Blood sugar. Lower blood sugar will delay the onset and slow the progression of diabetic retinopathy. Chronically high blood sugar and the longer the duration of diabetes, the more likely chance of that person having diabetic retinopathy.
- Medical conditions. People with high blood pressure and high cholesterol are at greater risk for developing diabetic retinopathy.
- Ethnicity. Hispanics, African Americans, and Native Americans are at greater risk for developing diabetic retinopathy.
- Pregnancy. Women with diabetes could have an increased risk of developing diabetic retinopathy during pregnancy. If they already have diabetic retinopathy, it might worsen during pregnancy.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

In light of the holiday season, here are our top 10 eye care jokes.
1) What do you call a blind deer? No Eye Deer!
2) What do you call a blind deer with no legs? Still No Eye Deer!
3) Why do eye doctors live long lives? Because they dilate!
4) Why did the blind man fall into the well? He couldn’t see that well.
5) Why shouldn’t you put avocados on your eyes? Because you might get guac-coma!
6) What did the right eye say to the left eye? "Between you and me, something smells."
7) A man goes to his eye doctor and tells the receptionist he’s seeing spots. The receptionist asks if he’s ever seen a doctor. The man replies, “No, just spots.”
8) How many eye doctors does it take to screw in a light bulb? One … or two
9) Unbeknownst to her, a woman was kicked out of peripheral vision club. She didn’t see that one coming!
10) What do you call a blind dinosaur? A do-you-think-he-saurus
Bonus: What do you call a blind dinosaur’s dog? A do-you-think-he-saurus rex!
Article contributed by Dr. Jonathan Gerard

Punctal plugs are something we use to help treat Dry Eye Syndrome.
This syndrome is a multifactorial problem that comes from a generalized decrease in the amount and quality of the tears you make. There is often both a lack of tear volume and inflammation in the tear glands, which interfere with tear production and also cause the quality of the tears to not be as good.
We make tears through two different mechanisms. One is called a basal secretion of tears, meaning a constant low flow or production of tears to keep the eye moist and comfortable. There is a second mechanism called reflexive tear production, which is a sudden flood of tears caused by the excitation of nerves on the eye surface when they detect inflammatory conditions or foreign body sensations. It is a useful reflexive nerve loop that helps wash out any foreign body or toxic substance you might get in the eye by flooding the eye with tears. Consider what happens when you get suntan lotion in your eye. The nerves detect the irritation that the lotion creates, and your eyes quickly flood with tears.
That reflex mechanism is how some people get tearing even though the underlying cause of that tearing is dry eye. They don’t produce enough of the basal tears, the eye surface gets irritated and then the reflex tearing kicks in and floods their eyes, tearing them up. Once that reflex is gone then the eye dries out again and the whole cycle starts over.
One of the treatments for dry eyes is to put a small plug into the tear drainage duct so that whatever tears you are making stay on the eye surface longer instead of draining away from the eye into to the tear drainage duct and emptying into your nose.
There are several different types of punctal plugs. Some are made of a material that is designed to dissolve over time. Some materials dissolve over two weeks, while others can last as long as 6 months. There are also plugs made out of a soft silicone material that are designed to stay in forever. They can, however, be removed fairly easily if desired or they can fall out on their own, especially if you have a habit of rubbing near the inside corner of your eye.
One of the big advantages of punctal plugs is that they can improve symptoms fairly rapidly - sometimes as quickly as a day.
The long-term medical treatment for dry eyes such as Restasis, Xiidra or the vitamin supplement HydroEye can take weeks or months to have a good effect.
On the other hand, plugs simply make you retain your tears for a longer time; they don’t help the underlying inflammation. That is where the medical treatment comes in. Sometimes it is useful to use a temporary plug for more instant relief while you are waiting for the medical treatment to work. Sometimes there is clearly just a deficiency of tears and not much inflammation and the plugs alone will improve your symptoms.
All in all, punctal plugs are a safe, effective, and relatively easily-inserted treatment for dry eyes.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

